Child and Adolescent Psychiatry
Session: Poster Session
(036) The Virginia Mental Health Access Program (VMAP): A New Frontier for Pediatric C-L Psychiatry
Trainee Involvement: No

Mary Lynn Dell, MD, DMin, MHA (she/her/hers)
Professor of Psychiatry & Neurobehavioral Sciences
University of Virginia
Richmond, Virginia, United States
Rachel Reynolds, n/a
VMAP State Operations Manager
Medical Society of Virginia Foundation
Richmond, Virginia, United States- MM
Matthew McKinney, n/a
Data Analyst & Evaluator
Medical Society of Virginia Foundation
Richmond, Virginia, United States - BS
Bela Sood, MD MSHA, MD MSHA
Senior Professor child mental health policy
Virginia Commonwealth University Richmond VA
Midlothian, Virginia, United States
Presenting Author(s)
Co-Author(s)
Results/ American Academy of Pediatrics (2022). Recommendations for Preventive Pediatric Health Care. https://downloads.aap.org/AAP/PDF/periodicity_schedule.pdf Delamater, A. M., Guzman, A., & Aparicio, K. (2017). Mental health issues in children and adolescents with chronic illness. International Journal of Human Rights in Healthcare, 10(3), 163-173. https://doi.org/10.1108/IJHRH-05-2017-0020 Lauerer J.A., Marenakos, K.G., Gaffney, K., Ketron, C., & Huncik, K. (2018). Integrating behavioral health in the pediatric medical home. Journal of Child and Adolescent Psychiatric Nursing, 31, 39-42. https://doi.org/10.1111/jcap.12195
Background: Virginia faces challenges in supporting mental health needs of children and adolescents with chronic, comorbid health conditions. Mental health concerns in individuals under 21 years of age are often under-identified (AAP, 2022). Individuals with chronic illness are identified as having much higher risk for experiencing a comorbid mental health challenge (Delameter et al., 2017). While integrated care is the goal, it is often challenging to develop and maintain in smaller practice settings (Lauerer et al., 2018). Virginia ranked 48th in the US for access to youth mental health services in 2022.
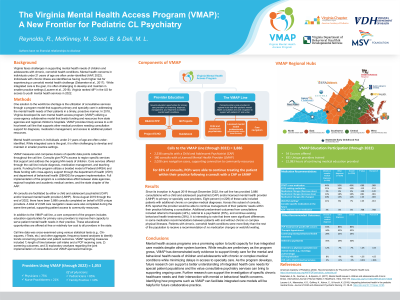
Methods: One solution to the workforce shortage is the utilization of consultative services through a program model that supports primary and specialty care in addressing the mental health needs of their patients in a timely, proactive manner. In 2018, Virginia developed its own mental health access program (VMAP) utilizing a cross-agency collaborative model that braids funding and resources from state agencies and regional children’s hospitals. VMAP provides timely access to a 40 hour/week call line that supports other medical providers needing consultation support for diagnosis, medication management, and access to additional patient resources.
Discussion: Since its inception in August 2019 through December 2022, the call line has provided 2,799 consultations with a child and adolescent psychiatrist (CAP) and/or licensed mental health provider (LMHP) to primary or specialty care providers. Eight percent (n=229) of these calls included patients with additional chronic or complex medical diagnoses. Across this subset of consults, 83% reported the provider would be able to continue management of their patients’ needs within their practice following a consultation. Additional predominant outcomes from consultations included referral to therapists (44%), referral to a psychiatrist (35%), and continue existing behavioral health treatments (28%). It is interesting to note that there were significant differences in some medication recommendations between patients with and without chronic or complex physical illnesses. Patients with chronic, comorbid health conditions were more likely than the rest of the population to receive a recommendation of no medication changes or watchful waiting.
Conclusions: Mental health access programs are a promising option to build capacity for true integrated care models despite other system barriers. While results are preliminary as the program grows, VMAP has demonstrated early evidence to support timely care for the mental and behavioral health needs of children and adolescents with chronic or complex medical conditions while minimizing delays in access to specialty care. As the program develops, future research can support a better understanding of integrated health care needs for special patient populations and the value consultative psychiatry services can bring to supporting ongoing care.
References:

