Collaborative and Integrated Care
Session: Poster Session
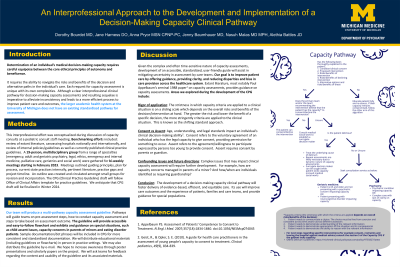
(051) An Interprofessional Approach to the Development and Implementation of a Decision-making Capacity Clinical Pathway
Trainee Involvement: No

Jane Harness, DO (she/her/hers)
Clinical Assistant Professor
University of Michigan
Ann Arbor, Michigan, United States
Nasuh Mahmoud Malas, MD, MPH (he/him/his)
Division Director and Service Chief, Child and Adolescent Psychiatry
University of Michigan
Ann Arbor, Michigan, United States
Dorothy Bourdet, MD
Clinical Instructor Child and Adolescent Consult-Liaison Psychiatry
University of Michigan
Ann Arbor, Michigan, United States- AP
Anna Pryor, MSN, CPNP-PC
Nurse Practitioner
Michigan Medicine
Ann Arbor, Michigan, United States - AB
Alethia J. Battles, JD
Associate General Counsel
University of Michigan - Michigan Medicine
Ann Arbor, Michigan, United States - JB
Jennifer Baumhauer, MD
Clinical Assistant Professor of Psychiatry
University of Michigan
Ann Arbor, Michigan, United States
Presenting Author(s)
Co-Author(s)
Background/Significance: Determination of an individual’s medical decision-making capacity requires careful equipoise between the core ethical principles of autonomy and beneficence. It also requires the ability to navigate the risks and benefits of the decision and alternative paths in the individual’s care. Each request for capacity assessment is unique with its own complexities. However, there are clear principles that can be applied widely to create a standardized, informed approach to the awareness of need for capacity assessments, elements necessary for completion of capacity assessments and subsequent pathways of care management after the assessment determinations. Therefore, having a clear interprofessional clinical pathway for decision-making capacity assessments and resulting sequelae is imperative to alleviate inconsistency and leads to a more efficient process to improve patient care and outcomes. The pathway development started due to a noted gap by the Pediatric Consultation-Liaison Psychiatry Service at a tertiary care, academic Children’s Hospital for young adults ages 18-25 who were refusing necessary cares. Further exploration demonstrated that the larger academic health system did not have an existing clinical pathway for capacity assessment. In order to develop a functional and efficient clinical pathway regarding clinical capacity assessment, we assembled an interprofessional team to review current literature [1], best practices, laws and gaps in current practices. A team of 18 people from child and adult psychiatry, internal medicine, pediatrics, nursing, social work, ethics and legal was assembled. Meetings started in March 2023 and occurred every 2 weeks. These meetings informed a working document, available for iterative revision, that was edited by the pathway lead team. We will describe the clinical pathway for capacity assessment and resulting sequelae, including a timely process to determine when legal action (like a court-appointed guardian) is indicated and necessary. We will also share the discrete steps taken to develop and implement the clinical pathway. It is important to have an accessible, user-friendly, standardized guide to decision making capacity assessments and resulting sequelae, given the time-sensitive nature, ramifications and complexity of these assessments. Identifying the need for a capacity assessment, empowering care teams to conduct straightforward assessments, consulting psychiatry if needed, and defining management algorithms depending on the determination of the capacity assessment is invaluable given how common and heterogeneous these assessments may be. Having such a policy will ameliorate unnecessary care-team stress and mitigate disparities and bias in care delivery and hopefully result in improved outcomes. It will also aid the patient’s and family’s experience by reducing care team uncertainty. Conclusion/Implications: We hope that the development of a decision-making capacity clinical pathway will foster delivery of evidence-based, efficient, and equitable care. We hope that it will improve care outcomes and the experience of patients, families and care teams. Future research in this area might include comparison of patient, family and care team experience in utilization of a clinical pathway, as well as identification of changes in patient outcomes following implementation of the pathway.
Methods:
Results:
Discussion:
References:

