Quality and Safety
Session: Poster Session
(170) Delivering Care and Communicating Bad News in the Age of Open Notes: When the Chart Shares Diagnoses Before the Doctor Can
Trainee Involvement: Yes

Vlad I. Velicu, MD
Psychiatry Resident at The Mount Sinai Hospital
Icahn School of Medicine at Mount Sinai
Kew Gardens, New York, United States.jpg)
Shruti Mutalik, MD (she/her/hers)
Transplant and Consultation Liaison Psychiatrist, Mount Sinai Hospital
Assistant Professor of Psychiatry, Icahn School of Medicine at Mount Sinai
Woodside, New York, United States- JA
Jacob M. Appel, MD, JD
Associate Professor of Psychiatry
Icahn School of Medicine at Mount Sinai
New York, New York, United States - EM
Ehsan Moazen-Zadeh, MD, MSc
Psychiatry Resident
Icahn School of Medicine
New York, New York, United States - CE
Carrie Ernst, MD
Director, CL Psychiatry Fellowship, Mount Sinai Hospital
Icahn School of Medicine at Mount Sinai
New Rochelle, New York, United States
Presenting Author(s)
Co-Author(s)
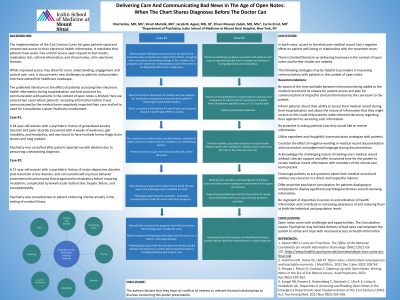
The implementation of the 21st Century Cures Act gave patients rapid and unrestricted access to their electronic health information. While improved access may allow for more understanding, engagement and control over care, it also presents new challenges to patients and providers that have altered the healthcare landscape. One challenge involves breaking bad news. We present two cases where patients’ accessing information before it was communicated by the medical team negatively impacted their care. Guided by these cases, we outline suggestions for delivering care and communicating bad news in the age of open notes. Cases: 1) A 21 year old woman with a psychiatric history of major depressive disorder, post-traumatic stress disorder, and non-suicidal self-injurious behavior presented with pneumonia that progressed to respiratory failure requiring intubation, complicated by biventricular dysfunction, hepatic failure, and encephalopathy. While in the rehabilitation unit, the patient accessed her hospital chart, leading to an increase in health-related anxiety, panic attacks and nightmares. Psychiatry was consulted for assistance with managing these symptoms. In both cases, access to the electronic record had a negative effect on patient well-being or relationship with the treatment team. There is limited literature on delivering bad news in the context of open notes and further studies are needed. More expedient and thoughtful communication between providers and patients is required (Posada, 2022). Other aspects to consider are proactively asking patients how they would like to receive information, the impact of negative wording in documentation (Hutchins, 2022), and disparities in access to and utilization of health information (Sangal, 2021). Open notes come with challenges and opportunities. The Consultation-Liaison Psychiatrist may facilitate delivery of bad news and empower the patient to utilize and cope with increased access to health information. Hutchins GPJ, Stone VE, Hall KT. Open notes: Unintended consequences and teachable moments. J Med Ethics. 2022 Dec 2:jme-2022-108765. Posada J, Potvin H, Cookson C. Opening Up with Open Notes: Writing Notes in the Era of Full Patient Access. Acad Psychiatry. 2022 Apr;46(2):259-263. Sangal RB, Powers E, Rothenberg C, Ndumele C, Ulrich A, Hsiao A, Venkatesh AK. Disparities in Accessing and Reading Open Notes in the Emergency Department Upon Implementation of the 21st Century CURES Act. Ann Emerg Med. 2021 Nov;78(5):593-598.
Background:
2) A 64 year old woman with a psychiatric history of generalized anxiety disorder and panic disorder presented with 4 weeks of weakness, gait instability, and headaches, and was found to have multiple hemorrhagic brain lesions and lung nodules. Psychiatry was consulted after the patient reported suicidal ideation due to presuming a devastating diagnosis. While awaiting the pathology report, which was delayed for 9 days, the Consultation-Liaison Psychiatry team helped to develop a multi-step plan to communicate the results. The pathology revealed metastatic neuroendocrine small cell cancer. Due to difficulty coordinating the plan to coincide with the results release, the patient read the report in MyChart before the medical team was able to inform her. She expressed anger and insisted upon a referral to another hospital for outpatient follow-up.
Discussion:
Conclusions:
References:

