Neurocognitive Disorders, Delirium, and Neuropsychiatry
Session: Poster Session
(092) "It's Not in My Head:" Diagnostic Challenges in Patients with Suspected Functional Neurological Disorders Across the Lifespan
Trainee Involvement: Yes

Kara Narzikul, MD
Resident Physician in Psychiatry & Family Medicine
University of Pittsburgh Medical Center
Pittsburgh, Pennsylvania, United States- NS
Neeta Shenai, MD
Visiting Associate Professor of Psychiatry
University of Wisconsin School of Medicine and Public Health
Madison, Wisconsin, United States 
Meredith Spada, MD, MEd
Assistant Professor of Psychiatry
University of Pittsburgh
Pittsburgh, Pennsylvania, United States- AJ
Anna Jolliffe, DO
Assistant Professor of Psychiatry
UPMC Western Psychiatric Hospital
Pittsburgh, Pennsylvania, United States .png)
Priya Gopalan, MD, FACLP (she/her/hers)
Associate Professor of Psychiatry
University of Pittsburgh Medical Center, Western Psychiatric Hospital
Pittsburgh, Pennsylvania, United States
Presenting Author(s)
Co-Author(s)
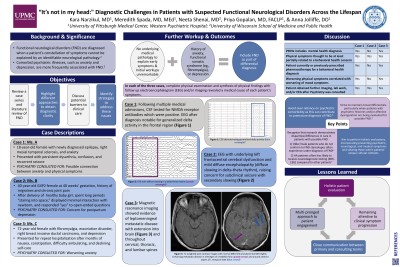
“It’s not in my head:” Diagnostic Challenges in Patients with Suspected Functional Neurological Disorders Across the Lifespan Background/Significance: Functional neurological disorders (FND) present across the lifespan and are diagnosed when a patient’s constellation of symptoms cannot be explained by an identifiable neurological pathology (Macchi, 2021). Psychiatric illnesses, such as anxiety and depression, are frequently associated with FND (Macchi, 2021). We present a literature review and three cases in which FND was initially the leading diagnosis, though in each case, full workup revealed a medical cause of presentation. Ms. A is an 18-year-old female with newly diagnosed epilepsy, right mesial temporal sclerosis, and anxiety who presented with persistent dysarthria, confusion, and recurrent seizure. Psychiatry was consulted to explore the possible connection between the patient’s anxiety and physical symptoms. Following multiple medical admissions, she was diagnosed with autoimmune encephalitis. Ms. B is a 40-year-old G4P2 female at 40 weeks' gestation with migraines and chronic joint pain who presented for repeat cesarean section. After delivery of a healthy baby girl, she spent long periods “staring into space,” displayed minimal interaction with her newborn, and responded “yes” to open-ended questions. Psychiatry was consulted due to concern for postpartum depression. An electroencephalogram ultimately demonstrated underlying left frontocentral cerebral dysfunction in addition to mild diffuse encephalopathy. Ms. C is a 72-year-old female with fibromyalgia, excoriation disorder, right breast invasive ductal carcinoma, and depression who presented for repeat hospitalization after months of nausea, constipation, difficulty ambulating, and declining self-care. Psychiatry was consulted for worsening anxiety. Magnetic resonance imaging showed leptomeningeal metastatic disease with extension into the brain and throughout all spinal levels. In each case, the differential diagnosis included FND, given the overlay of somatic symptoms and the preconceived association between FND and psychiatric comorbidity; however, complete physical examination as well as synthesis of physical findings with follow up electroencephalogram and/or imaging ultimately revealed a medical cause of each patient’s symptoms. Since somatoform disorders are the most prevalent psychiatric diagnoses in inpatient and outpatient neurology populations, and since studies have demonstrated disparities in the workup of patients with FND, the importance of holistic evaluation of patients’ presenting psychiatric, neurological, and medical symptoms within their unique cultural contexts cannot be overstated (Watson, 2019). Conclusion/Implications: Watson, C., Sivaswamy, L., Agarwal, R., Du, W., & Agarwal, R. (2019). Functional Neurologic Symptom Disorder in Children: Clinical Features, Diagnostic Investigations, and Outcomes at a Tertiary Care Children’s Hospital. Journal of Child Neurology, 34(6): 325-331.
Cases:
Discussion:
Close surveillance of clinical symptom progression, maintaining a broad differential, and a multi-pronged approach to patient engagement were instrumental in identifying the primary explanations for these patients’ presentations. The Consult-Liaison (CL) psychiatrist has a crucial role in evaluating patients with neurologic presentation and comorbid psychiatric illness, in identifying and working to address the influence of racial disparities in patients’ care, and in advocating for further workup when indicated.
References:
Macchi, Z.A., Kletenik, I., Olvera, C., & Holden, S.K. (2021). Psychiatric comorbidities in functional movement disorders: A retrospective cohort study. Movement Disorders Clinical Practice, 8(5): 725-732.

