Substance Use and Related Disorders
Session: Poster Session
(176) Multidisciplinary Management of Opioid Use Disorder in the Era of Fentanyl and Xylazine in the City of Brotherly Love
Trainee Involvement: Yes

Jasmine Miller, MPH
Student Researcher
Thomas Jefferson University-Sidney Kimmel Medical College
Philadelphia, Pennsylvania, United States- BV
Bethanne Venkatesan, n/a
Medical Student
Thomas Jefferson University Hospital
Philadelphia, Pennsylvania, United States 
Zahid Syed, MD
Physician Resident
Thomas Jefferson University Hospital
Philadelphia, Pennsylvania, United States- CF
Christopher Ferry, MD
Resident Physician
Thomas Jefferson University Hospital
Philadelphia, Pennsylvania, United States - NL
Nicolette Lee, MD
resident physician
Thomas Jefferson University Hospital
Philadelphia, Pennsylvania, United States 
Finola D. Mcnelis Goudy, n/a
Medical Student
Sidney Kimmel Medical College
Philadelphia, Pennsylvania, United States- CM
Carey Myers, MD, PhD
Attending Psychiatrist
Albert Einstein Medical Center
Philadelphia, Pennsylvania, United States - JL
Jahaira Lopez-Pastrana, MD
Assistant Professor of Psychiatry
Thomas Jefferson University Hospital
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Co-Author(s)
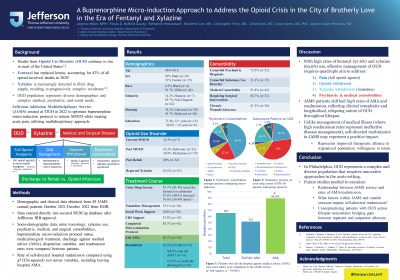
Background/Significance: Deaths from opioid use disorder continue to rise in most areas of the United States; fentanyl has largely replaced heroin and accounted for 82 % of all opioid-involved deaths in 2020. Moreover, xylazine is increasingly detected in the illicit drug supply resulting in a complex toxidrome. Consultation and Liaison (C-L) psychiatrists are vital in managing opioid use disorder. In 2022, the C-L Psychiatry department at Thomas Jefferson University Hospital developed Jefferson Addiction Multidisciplinary Service (JAMS) to optimize its buprenorphine microinduction protocol utilizing a multidisciplinary approach, including other medical specialties, social worker, and certified recovery specialist (CRS). Methods: Demographic and clinical data of patients for whom a JAMS consult was placed from October 2021-October 2022 were collected from the electronic medical record (EMR) and entered directly into secure database (REDCap) after Jefferson IRB approval. Socio-demographic data, urine toxicology, xylazine use, psychiatric and medical/surgical comorbidities, buprenorphine microinduction status, medical/surgical treatment, discharge against medical advice (AMA), and discharge disposition variables were compared between patients. Continuous variables were compared using a one-way analysis of variance (ANOVA), and categorical variables were compared using Chi-squared test across race/ethnicity on SPSS software. Discussion: Our results are consistent with national data, showing the prevalence of fentanyl/xylazine in OUD. However, fentanyl was not ordered in all cases, demonstrating the need to reinforce providers’ education. Tizanidine was used to manage xylazine withdrawal, recognizing the difference between opioids and xylazine withdrawal. Concomitant psychiatric disorders were managed during the hospitalization course, which helped to prevent behavioral and emotional disturbance from interfering with treatment. Patients received support from CRS and were seen by a social worker who provided another support layer and facilitated the opioid aftercare plan. Conclusion/Implications: JAMS provides services to a diverse population in Philadelphia independently of their socio-demographic backgrounds, medical insurance coverage, legal status, medical and psychiatric comorbidities, etc. A multidisciplinary approach to managing OUD in the era of fentanyl and xylazine is essential to improve the outcomes of established buprenorphine microinduction protocols. 1.Friedman J, Montero F, Bourgois P, et al. Xylazine spreads across the US: A growing component of the increasingly synthetic and polysubstance overdose crisis. Drug Alcohol Depend. 2022;233:109380. doi:10.1016/j.drugalcdep.2022.109380 2.Johnson, J; Pizzicato, L; Johnson, C; Viner, K. Increasing presence of xylazine in heroin and/or fentanyl deaths, Philadelphia, Pennsylvania, 2010-2019. 3. https://www.cdc.gov/drugoverdose/deaths/synthetic/index.html
Results: From 2021- 2022, fifty-two patients were seen by JAMS for buprenorphine microindution. So far, twenty-one patients have been analyzed, five (23.8%) identified as female and sixteen (76.2%) as male, nineteen (90.5%) identified as white, and two (9.52%) identified as African American. Twenty (95.2%) had concomitant substance use disorder, fourteen (66.6%) had concurrent psychiatric disorders, twelve (60.0%) required tizanidine for management of xylazine withdrawal, and seven (33.3%) had wounds. Seventeen of nineteen (89.4%) of the UDS samples were positive for opiates, but not all were tested for fentanyl. Ten (52.6%) UDS samples were positive for fentanyl. Sixteen (76.1%) finished the microinduction protocol, sixteen (76.1%) went to rehab, and five (23.8%) left AMA. Social workers evaluated all the patients, and twenty patients received CRS support.
References:

