Diversity, Equity, and Inclusion
Session: Poster Session
(069) Studying Inequities in Utilization of Psychiatric Consultation Services in a Women's Health Hospital
Trainee Involvement: Yes

H. Nur Eken, MD (she/her/hers)
Resident Physician
University of Pittsburgh Medical Center, Department of Psychiatry
Pittsburgh, Pennsylvania, United States
Meredith Spada, MD, MEd
Assistant Professor of Psychiatry
University of Pittsburgh
Pittsburgh, Pennsylvania, United States- SP
Sarah Pedersen, PhD
Associate Professor
University of Pittsburgh
Pittsburgh, Pennsylvania, United States .png)
Priya Gopalan, MD, FACLP (she/her/hers)
Associate Professor of Psychiatry
University of Pittsburgh Medical Center, Western Psychiatric Hospital
Pittsburgh, Pennsylvania, United States
Presenting Author(s)
Co-Author(s)
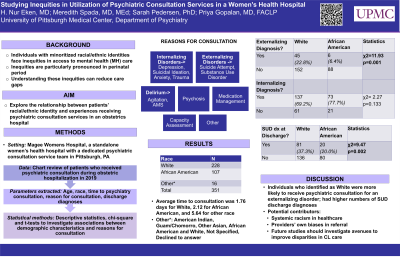
Background: Individuals with minoritized racial and ethnic identities face inequities in access to mental health care, particularly in the perinatal period, as psychiatric disorders are a major contributor to maternal mortality.1 Moreover, an observed increase in perinatal psychiatric disorders during the COVID-19 pandemic further exacerbated inequities in access to mental health care for patients of color.2 In this study, we aimed to explore the potential relationship between patients’ racial/ethnic identity and experiences when receiving psychiatric consultation services in an obstetrics hospital.
Methods: We analyzed data from patients who received psychiatric consultation during obstetric hospitalization in 2019. Specifically, we looked at demographic variables, time to psychiatry consultation, reason for consultation and discharge diagnoses. We used descriptive statistics, chi-square analyses and t-tests to investigate associations between demographic characteristics and reasons for consultation.
Results: We analyzed data from 351 patients assigned female at birth with race/ethnicity extracted from medical record (White =228, African American=107, Other (American Indian, Guam/Chomorro, Other Asian, African American and White, Not Specified, Declined (to answer)=16). We found that the average time to consultation was 1.76 days for White, 2.12 for African American, and 5.64 for “Other”. We categorized reasons for consults based on disease process: internalizing (depression, anxiety, trauma-related disorders, suicidal ideation), externalizing (substance use disorders (SUDs), suicide attempts), psychosis, delirium (including agitation, AMS), capacity assessment, medication management and “other.” No significant difference was found between individuals identifying as White or African American with internalizing diagnoses (majority depression and anxiety, p=0.13); however, individuals who identified as White (n=45/197) were significantly more likely to be given an externalizing (majority SUD) diagnosis compared to those identifying as Black (n=6/94, p=0.001). Individuals who identified as White were also more likely to carry an alcohol and substance use disorder diagnoses at discharge (81/136) compared to those identifying as African American (20/80, p=0.002).
Discussion: Individuals who identified as White were more likely to receive psychiatric consultation for an externalizing disorder and had significantly higher numbers of SUD diagnoses upon discharge compared to individuals who identified as Black. Potential reasons include individuals from minoritized populations hesitating to discuss substance use with providers due to fear related to historical injustices and systemic racism in healthcare, which are particularly pertinent in the perinatal period. Another possibility is providers’ own biases in referral for SUD care. Limitations include small sample size for racial and ethnic groups other than White and African American.Implications: Future studies should investigate other contributors to disparities in access to care, as well as avenues to improve disparities in the inpatient care setting and beyond.
References:

