Catatonia
Session: Poster Session
(020) Unique Case to Treat Catatonia in Lithium Toxicity Resistant to Benzodiazepines
Trainee Involvement: Yes

Lauren Vicente, MD
Resident Psychiatrist
Zucker Hillside Hospital at Northwell/Hofstra
Staten Island, New York, United States- HS
Humaira Shoaib, MD
Consultation-Liaison Psychiatrist
Long Island Jewish Medical Center, Northwell Health
New Hyde Park, New York, United States 
Xavier Jimenez, MD, MA, FACLP
Director, Consultation Liaison Psychiatry
Long Island Jewish Medical Center (Northwell)
New Hyde Park, New York, United States- SG
Samuel Greenstein, MD
Director, Consultation-Liaison Psychiatry Fellowship
Long Island Jewish Medical Center - Northwell Health
New Hyde Park, New York, United States 
Shamik Mukherji, MD
Consultation-Liaison Psychiatrist, Psycho-Oncologist
Long Island Jewish Medical Center / Northwell Health
Queens, New York, United States- SS
Sohag Sanghani, MD, FAAGP, MPH
Director, ECT Service. Asst Professor
Zucker School of Medicine at Hofstra/Northwell
Glen Oaks, New York, United States - GP
Georgios Petrides, MD
Director Division of ECT, Zucker Hillside Hospital,
Northwell Health System
New York, New York, United States
Presenting Author(s)
Co-Author(s)
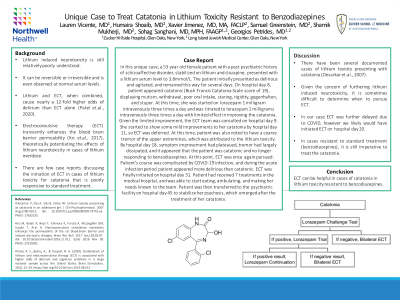
Background: Lithium induced neurotoxicity is still relatively poorly understood. It can be reversible or irreversible and is even observed at normal serum levels. Electroconvulsive therapy (ECT) transiently enhances the blood brain barrier permeability (Ito et.al., 2017), theoretically potentiating the effects of lithium neurotoxicity in cases of lithium overdose. There are few case reports discussing the initiation of ECT in cases of lithium toxicity for catatonia that is poorly responsive to standard treatment. Case: In this unique case, a 53 year old female patient with a past psychiatric history of schizoaffective disorder, stabilized on lithium and clozapine, presented with a lithium serum level to 3.8mmol/L. The patient initially presented as delirious and agitated, and remained this way for several days. On hospital day 8, patient appeared catatonic (Bush Francis Catatonia Scale score of 19), displaying mutism, withdrawal, poor oral intake, staring, rigidity, gegenhalten, and stupor. At this time, she was started on lorazepam 1 milligram intravenously three times a day and was titrated to lorazepam 2 milligrams intravenously three times a day with limited effect in improving the catatonia. Given the limited improvement, the ECT team was consulted on hospital day 9. She started to show some mild improvements to her catatonia by hospital day 11, so ECT was deferred. At this time, patient was also noted to have a coarse tremor of the upper extremities, which was attributed to the lithium toxicity. By hospital day 18, symptom improvement had plateaued, tremor had largely dissipated, and it appeared that the patient was catatonic and no longer responding to benzodiazepines. At this point, ECT was once again pursued. Patient’s course was complicated by COVID-19 infection, and during the acute infection period patient appeared more delirious than catatonic. ECT was finally initiated on hospital day 31. Patient had received 7 treatments in the medical hospital, and was able to start eating, ambulating, and making her needs known to the team. Patient was then transferred to the psychiatric facility on hospital day 45 to stabilize her psychosis, which emerged after the treatment of her catatonia. Discussion: There have been several documented cases of lithium toxicity presenting with catatonia (Desarkar et.al., 2007). Given the concern of furthering lithium induced neurotoxicity, it is sometimes difficult to determine when to pursue ECT. . In our case ECT was further delayed due to COVID, however we likely would have initiated ECT on hospital day 20. In cases resistant to standard treatment (benzodiazepines), it is still imperative to treat the catatonia. Conclusion: ECT can be helpful in cases of catatonia in lithium toxicity resistant to benzodiazepines. References Desarkar P, Das A, Das B, Sinha VK. Lithium toxicity presenting as catatonia in an adolescent girl. J Clin Psychopharmacol. 2007 Aug;27(4):410-2. doi: 10.1097/01.jcp.0000280309.73742.aa. PMID: 17632235. Ito M, Bolati K, Kinjo T, Ichimura K, Furuta A, McLoughlin DM, Suzuki T, Arai H. Electroconvulsive stimulation transiently enhances the permeability of the rat blood-brain barrier and induces astrocytic changes. Brain Res Bull. 2017 Jan;128:92-97. doi: 10.1016/j.brainresbull.2016.11.011. Epub 2016 Nov 30. PMID: 27915091.

