Substance Use and Related Disorders
Session: Poster Session
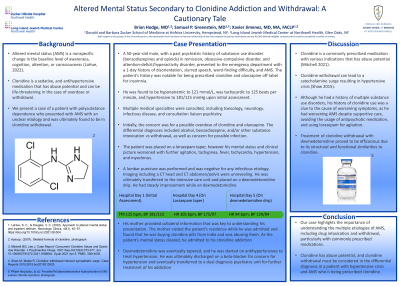
(173) Altered Mental Status Secondary to Clonidine Addiction and Withdrawal: A Cautionary Tale
Trainee Involvement: Yes

BRIAN HODGE, MD (he/him/his)
Psychiatry Resident
Zucker Hillside Hospital
Jamaica, New York, United States- SG
Samuel Greenstein, MD
Director, Consultation-Liaison Psychiatry Fellowship
Long Island Jewish Medical Center - Northwell Health
New Hyde Park, New York, United States 
Xavier Jimenez, MD, MA, FACLP
Director, Consultation Liaison Psychiatry
Long Island Jewish Medical Center (Northwell)
New Hyde Park, New York, United States
Presenting Author(s)
Co-Author(s)
1. LaHue, S. C., & Douglas, V. C. (2022). Approach to altered mental status and inpatient delirium. Neurologic Clinics, 40(1), 45–57. https://doi.org/10.1016/j.ncl.2021.08.004 2. Mitchell BG, Lee J. 3. 2. Shaw M, Matsa R. Clonidine withdrawal induced sympathetic surge. Case Reports 2015;2015:bcr2015210325
Background: Altered mental status (AMS) is a nonspecific change in the baseline level of awareness, cognition, attention, or consciousness (LaHue, 2022). One common etiology of AMS is drug intoxication or withdrawal. Clonidine, a sedative and antihypertensive medication, has abuse potential, and can be life-threatening in the case of overdose or withdrawal. We present a case of a patient with polysubstance dependence who presented with AMS with an unclear etiology and was ultimately found to be in clonidine withdrawal.
Case: A 50-year-old male, with a past psychiatric history of substance use disorder (benzodiazepines and opioids) in remission, obsessive-compulsive disorder, and attention-deficit/hyperactivity disorder, presented to the emergency department with a 1-day history of disorientation, slurred speech, word-finding difficulty, and AMS. He was found to be hyponatremic to 121 mmol/L. The patient’s history was notable for being prescribed clonidine and olanzapine off-label for insomnia. Multiple medical specialties were consulted, including toxicology, neurology, and consultation liaison psychiatry. Initially, the concern was for a possible overdose of clonidine and olanzapine. Even though he was eventually placed on scheduled lorazepam, his mental status and clinical picture worsened with further agitation, tachypnea, fever, tachycardia, hypertension, and myoclonus. He was ultimately transferred to the intensive care unit. and placed on a dexmedetomidine drip. He had steady improvement while on dexmedetomidine. His mother found out that he was buying clonidine pills from India and abusing them. As the patient’s mental status cleared, he too admitted to his clonidine addiction. Dexmedetomidine was eventually tapered, and he was started on antihypertensives to treat possible hypertension. He was ultimately discharged on a beta-blocker for concern for hypertension and eventually transferred to a dual diagnosis psychiatry unit for further treatment of his addiction.
Discussion: Clonidine is a commonly prescribed medication with various indications that has abuse potential (Mitchell 2021). Clonidine withdrawal can lead to a catecholamine surge resulting in hypertensive crisis (Shaw 2015). In this patient, AMS was initially thought to be secondary to hyponatremia. Although he had a history of multiple substance use disorders, his history of clonidine use was a clue to the cause of worsening symptoms, as he had worsening AMS despite supportive care, avoiding the usage of antipsychotic medication, and using lorazepam for agitation. Treatment of clonidine withdrawal with dexmedetomidine proved to be efficacious due to its structural and functional similarities to clonidine.
Conclusion: Our case highlights the importance of understanding the multiple etiologies of AMS, including drug intoxication and withdrawal, particularly with commonly prescribed medications. Clonidine has abuse potential, and clonidine withdrawal must be considered in the differential diagnosis in a patient with hypertensive crisis and AMS.
References:
Case Report: Concurrent Clonidine Abuse and Opioid Use Disorder. J Psychoactive Drugs. 2021 Sep-Oct;53(4):373-377. doi: 10.1080/02791072.2021.1908644. Epub 2021 Apr 5. PMID: 33814003.

