Cardiology
Session: Poster Session
(005) Delusional Parasitosis and the Urgent Need for a Ventricular Assist Device
Trainee Involvement: Yes

Minhi Kang, MD (she/her/hers)
Resident
Rutgers Robert Wood Johnson
New Brunswick, New Jersey, United States
Rahul S. Ramasubramani, MD
Psychiatry Resident
Rutgers Robert Wood Johnson
Piscataway, New Jersey, United States
Shawen Ilaria, MD
Assistant Professor
Rutgers RWJMS
New Brunswick, New Jersey, United States- AT
Anthony Tobia, MD
Professor of Psychiatry
Rutgers Robert Wood Johnson Medical School
franklin Park, New Jersey, United States 
Adam Trenton, DO
Associate Professor of Psychiatry
Rutgers Robert Wood Johnson Medical School
NEW BRUNSWICK, New Jersey, United States
Presenting Author(s)
Co-Author(s)
Conclusions/Implications: With appropriate psychiatric treatment and multidisciplinary collaboration, the presence of a psychotic disorder need not preclude a patient from undergoing VAD placement.
Background: Psychosocial evaluation, sometimes including psychiatric consultation, is recommended (Caro, 2016) in the preoperative work-up for ventricular assist devices (VAD). Sometimes there is a call for consultation-liaison (CL) psychiatrists to provide ongoing care in advance of VAD placement, as this case report exemplifies.
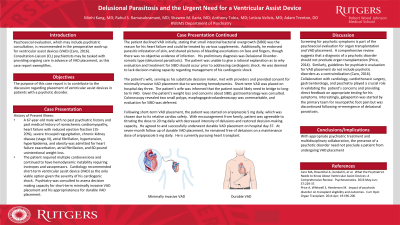
Case: A 67-year-old man was admitted for advanced heart failure (ejection fraction 15-20%), atrial fibrillation, and 40-lb unintentional weight loss. Cardiology recommended placing a short-term VAD and advised the patient that a long-term VAD would likely follow. Psychiatry was consulted for clearance. The patient was reluctant about VAD placement because he believed that he had small intestinal bacterial overgrowth (SIBO), that SIBO caused his heart failure, and that if SIBO were treated his heart failure would improve without need for a VAD. Further, he reported parasitic infestation of his skin, noting that he had evidence in the form of pictures and skin samples. He had no history of psychiatric illness or cognitive decline, and had been a successful business owner until heart failure forced him to retire. Several years prior he contracted Lyme disease, and subsequently became preoccupied with concern of acquiring other infections and developed an interest in natural remedies, of which he was using several. He was diagnosed with Delusional disorder, somatic type (delusional parasitosis) and determined to lack decision-making capacity for VAD placement. There was concern about starting an antipsychotic given his prolonged QTc interval (593 milliseconds), but also risk in delaying treatment as he was unwilling to receive a VAD and his condition was declining. Cardiothoracic surgery was hesitant to place a VAD in a patient displaying psychosis and lacking decision-making capacity. With encouragement from his family, he agreed to start aripiprazole and was titrated to 20 mg daily. Extensive collaboration was required between cardiology, cardiothoracic surgery, gastroenterology, and psychiatry. Providers validated the patient’s concerns (e.g. significant weight loss), and provided direct feedback about which tests were appropriate (e.g. colonoscopy to rule out colorectal cancer) and which were not (e.g. jejunal aspirate culture to rule out SIBO). The patient responded well to aripiprazole and support from the psychiatry team and the intensity of his delusions waned and his decision-making capacity was restored. He underwent successful placement of a short-term VAD, and later was transitioned to a long-term device.
Discussion: Screening for psychotic symptoms is part of the psychosocial evaluation for organ transplantation and VAD placement. A comprehensive review (Price, 2014) suggests that a diagnosis of psychotic disorder should not preclude organ transplantation. Similarly, guidelines for psychiatric evaluation for VAD placement (Caro, 2016) do not include psychotic disorders as a contraindication.
References:
1. Caro MA, Rosenthal JL, Kendall K, et al.: What the Psychiatrist Needs to Know About Ventricular Assist Devices: A Comprehensive Review. Psychosomatics. 2016; 57: 229-37.
2. Price A, Whitwell S, Henderson M. Impact of psychotic disorder on transplant eligibility and outcomes. Curr Opin Organ Transplant. 2014; 19: 196-200.

