Quality and Safety
Session: Poster Session
(165) Ethical Implications in Assessment of a Patient Reporting Sexual Assault: A Case Report and Discussion
Trainee Involvement: Yes
- MS
Maria F. Sarmiento, DO (she/her/hers)
Resident
UMass-Chan Baystate
Springfield, Massachusetts, United States 
Deepika Sundararaj, MD
Consultation-Liaison Psychiatry
UMass Chan Medical School - Baystate Medical Center
Bloomfield, Connecticut, United States
Presenting Author(s)
Co-Author(s)
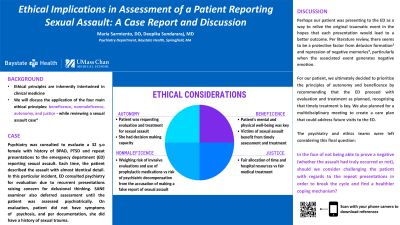
Ethical principles are inherently intertwined in clinical medicine. This report will discuss the application of the four main ethical principles - beneficence, nonmaleficence, autonomy, and justice - while reviewing a sexual assault case (Varkey, 2021) including the challenges, ethical conflicts and eventual resolution of the case. Perhaps our patient was presenting to the ED as a way to relive the original traumatic event in the hopes that each presentation would lead to a better outcome. Per literature review, there seems to be a protective factor from delusion formation (Gunn, 2018) and repression of negative memories (Otgaar, 2022), particularly when the associated event generates negative emotion. Given the case’s complexity, we used the four main ethical principles to guide our management: Autonomy: our patient was requesting examination and treatment for sexual assault and she had the decision-making capacity to do so Beneficence: patient’s mental and physical well-being was key and victims of sexual assault benefit from timely assessment and treatment Nonmaleficence: weighing the risk of invasive evaluations and multiple doses of prophylactic medications with the risk of psychiatric decompensation from the accusation of making a false report of sexual assault Justice: fair allocation of time and hospital resources vs fair treatment to which the patient is entitled For our patient, we ultimately decided to prioritize the principles of autonomy and beneficence by recommending that the ED proceed with evaluation and treatment as planned, recognizing that timely treatment is key. We also planned for a multidisciplinary meeting to create a care plan that could address future visits to the ED. The psychiatry and ethics teams were left considering this final question: in the face of not being able to prove a negative (whether the assault had truly occurred or not), should we consider challenging the patient with regards to the repeat presentations in order to break the cycle and find a healthier coping mechanism? When consulted on complex clinical cases, ethical concepts can help further examine the case and guide management and recommendations.
Background:
Case: Psychiatry was consulted to evaluate a 32yo female with history of BPAD, PTSD and repeat presentations to the emergency department (ED) reporting sexual assault. Each time, the patient described the assault with almost identical detail. In this particular incident, ED consulted psychiatry for evaluation due to recurrent presentations raising concern for delusional thinking. SANE examiner also deferred assessment until the patient was assessed psychiatrically. On evaluation, patient did not have symptoms of psychosis, and per documentation, she did have history of sexual trauma.
Discussion:
Conclusion:
References:
Bowdler, M; Kent, H. AMA J Ethics. 2018;20(1):36-43.
Gunn, R., Bortolotti, L. Can delusions play a protective role?. Phenom Cogn Sci 2018; 17, 813–833.
Otgaar, H., Howe. M., and Patihis, L. What science tells us about false and repressed memories, Memory, 2022; 30:1, 16-21.
Varkey B. Principles of Clinical Ethics and Their Application to Practice. Med Princ Pract. 2021;30(1):17-28.

