Collaborative and Integrated Care
Session: Poster Session
(042) Functional Coma in a 26-year-old Male Veteran
Trainee Involvement: Yes

Akpene Sarah Agamah, MPH, MBA, MD (she/her/hers)
Resident Physician
Loyola University Medical Center
Chicago, Illinois, United States- GN
GULAM NOORANI, MD, MPH
Attending Psychiatrist CL Psychiatry and Assistant Professor of Psychiatry
Hines VA
Chicago, Illinois, United States
Presenting Author(s)
Co-Author(s)
Introduction:
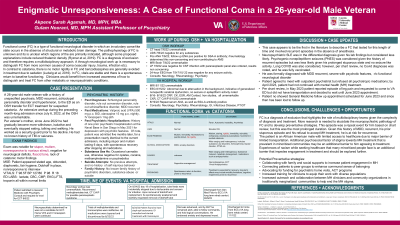
Functional coma (FC) is a type of functional neurological disorder in which an involuntary coma-like state occurs in the absence of structural or metabolic brain damage (Ryznar et al, 2019). In contrast to catatonia, there is no motor rigidity in FC and benzodiazepines are generally avoided in treatment due to sedation (Ludwig et al, 2016). In FC, vitals are stable and there is a spontaneous return to baseline functioning. Clinicians would benefit from increased awareness of how to distinguish and treat FC from other metabolic or neuropsychiatric conditions.
Case Presentation:
A 26-year-old male veteran with a history of schizotypal personality disorder and unspecified psychosis presents to the ED as an OSH transfer for ECT treatment for suspected catatonia. An extensive workup during the preceding month-long admission at the OSH was unremarkable aside from a positive ANA and an ENA panel positive for SSA-A antibody, which rheumatology determined as non-concerning.
Exam was notable for stupor, mutism, and lack of catatonic motor findings. All labs, vitals, and diagnostic exams were within normal limits. Neuropsychiatry determined he was not a candidate for ECT, as catatonia was less likely. He was continued on home doses of lorazepam and valproic acid with minimal change in presentation. The neurology team's assessment and workup was unremarkable. Trials of methylphenidate and bromocriptine were ineffective. On day 13, his course was complicated by staph epi bacteremia, which was treated with vancomycin.
Further chart review indicated that a year prior to presentation, he had two psychiatric hospitalizations: one for depression with psychotic features and another, five months later, for a presentation nearly identical to the current admission, with spontaneous recovery after stopping all medications. During this hospitalization, all medications were tapered and discontinued. On day 18 of hospitalization, tube feeds were incidentally stopped due to tachycardia, after which he became alert and oriented. He was able to tolerate a general diet, work with PT and OT and was discharged after day 20 to the inpatient rehabilitation unit.
Discussion:
This case is the first in the literature to describe a FC that lasted for this length of time and involved recurrent episodes in the absence of anesthesia. Neuropsychiatric SLE was in the differential diagnosis given his lab findings, but considered less likely. Psychogenic nonepileptiform seizures (PNES) was considered given the history of recurrent episodes, but was less likely given his prolonged stuporous state. Long COVID was also considered, however, per chart review, no Covid diagnoses was noted, and he was fully vaccinated.
Conclusion:
FC is a diagnosis of exclusion that highlights the role of multidisciplinary teams given the complexity of diagnosis and treatment. More research is needed to elucidate the neuropsychiatric pathology of FC and to develop preventative strategies.
References:
Ryznar E, Wilcox D. Functional Coma: Two Case Reports and a Review of the Literature. Psychosomatics. 2019 Jul-Aug;60(4):343-351. doi: 10.1016/j.psym.2019.03.005. Epub 2019 Mar 27. PMID: 31053419. Ludwig L, McWhirter L, Williams S, Derry C, Stone J. Functional coma. Handb Clin Neurol. 2016;139:313-327. doi: 10.1016/B978-0-12-801772-2.00028-X. PMID: 27719852.

