Collaborative and Integrated Care
Session: Poster Session
(058) Improving Colorectal Cancer Screening for Individuals with Severe Mental Illness in a Canadian Mental Health Hospital
Trainee Involvement: No
- SS
Sanjeev Sockalingam, MD, FACLP
Physician-in-Chief, VP Education, Professor
CAMH & University of Toronto
Toronto, Ontario, Canada - TT
Tania Tajirian, MD, FCFP
Chief of Hospital Medicine & Chief Medical Information Officer
Centre for Addiction and Mental Health
Toronto, Ontario, Canada 
Cristina de Lasa, MD, CCFP (COE)
Medical Head
Centre for Addiction and Mental Health
Toronto, Ontario, Canada- EM
Elnathan Mesfin, MSc
Research Coordinator
Centre for Addiction and Mental Health
Toronto, Ontario, Canada - VS
Vicky Stergiopoulos, MD FRCPC MHSc
Clinician Scientist
Centre for Addiction and Mental Health
Toronto, Ontario, Canada
Presenting Author(s)
Co-Author(s)
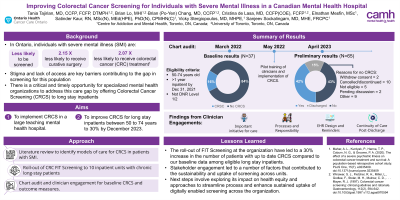
Background/Significance: Access to appropriate physical and preventative health care continues to be a critical challenge for individuals with severe mental illness. In particular, when it comes to colorectal cancer screening, this population has been found to have a relatively lower screening rate and poorer prognosis than the general population. In Ontario, individuals with severe mental illness (SMI) are less likely to be screened, 2.15 times less likely to receive potentially curative surgical treatment, and 2.07 times less likely to receive treatment for colorectal cancer (CRC). Thus, there is a need to look at alternative approaches to support colorectal cancer screening for this population.
Recently, there is growing interest in delivering screening within specialized mental health settings. Given that these organizations are the ‘de facto’ home for this stigmatized and vulnerable population, supporting the delivery of screening within these setting can be a very valuable approach for supporting these individuals.
Methods: This presentation outlines the findings of a QI project focused on piloting the roll-out of FIT screening to chronic inpatients at a mental health hospital in Toronto, Ontario. Over an 8-month period, a co-design approach was used to iteratively roll-out FIT test to units with eligible patients.
Results: As of December 2022, FIT screening rates have increased by 40% at the organization. Some of the lessons learned and recommendations that are critical for the success of this QI project include establishing close engagement and partnership with both hospitalists and nurses on the units. The electronic health record was also found to be important for helping hospitalists determine eligibility and setting reminders for the next screening.
Discussion: To date, this is the first study looking at how colorectal cancer screening can be implemented in specialized mental health settings to support individuals with severe mental illness. Future work should focus on exploring how this model can be scaled to other organizations and ways to expand this to other types of cancer screening.
Conclusion/Implications: This project outlines a way to support the physical and preventative health of individuals with severe mental illness across the lifespan. This work will have strong implications for consultation-liaison psychiatry in considering the comprehensive care of individuals from a mental health perspective.
Mahar, A. L., Kurdyak, P., Hanna, T. P., Coburn, N. G., & Groome, P. A. (2020). The effect of a severe psychiatric illness on colorectal cancer treatment and survival: A population-based retrospective cohort study. PLoS One, 15(7), e0235409. Protani, M., Alotiby, M., Seth, R., Lawrence, D., Jordan, S., Logan, H., . . . Kisely, S. (2022). Colorectal cancer treatment in people with severe mental illness: A systematic review and meta-analysis. Epidemiology and Psychiatric Sciences, 31, E82. doi:10.1017/S2045796022000634
References:

