Training and Education
Session: Poster Session
(196) Interdisciplinary Psychiatric Education: Enhancing Knowledge, Bridging Gaps, Improving Outcomes
Trainee Involvement: Yes
Stephen Marcoux, MD
Consultation-Liaison Psychiatry Fellow
University of Chicago Medical Center
Chicago, Illinois, United States- mt
marie B. tobin, MD, FACLP
Professor of Psychiatry
University of Chicago
chicago, Illinois, United States - SK
Shivani Kumar, MD
Assistant Professor of Psychiatry
University of Chicago Medicine
Chicago, Illinois, United States
Presenting Author(s)
Co-Author(s)
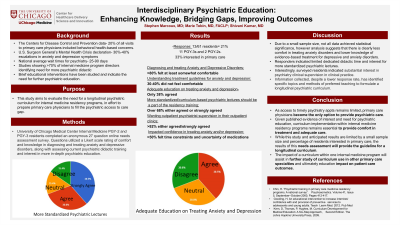
Background: The Centers for Disease Control and Prevention data indicates that 20% of all visits to primary care physicians included behavioral health-based concerns. Per the U.S. Surgeon General’s Mental Health Crisis declaration, there are 30%-40% escalations in anxiety and depression symptoms in teenagers and adults. National average wait times to see a psychiatrist are >25 days. ACGME guidelines for internal medicine residency programs do not require specific mental health curriculum, with studies showing >70% of internal medicine program directors identifying more psychiatric didactic is needed for their residents. Brief educational interventions have been studied and indicate the need for further psychiatric education. This study aims to evaluate the need for a longitudinal psychiatric curriculum for internal medicine residency programs, in effort to prepare primary care physicians to fill the psychiatric access to care gap.
Methods: University of Chicago Internal Medicine PGY-2 and PGY-3 residents will be assessed regarding their comprehension and comfort with treating and diagnosing anxiety and depressive disorders. A twenty-seven question online needs assessment survey is currently underway and will be analyzed May 2023. The results from the survey will be utilized to formulate a targeted year-long curriculum which will encompass multiple educational strategies.
Results: The results of the needs assessment survey have not been finalized, however I do attest that I will have the data of the survey completed prior to the ACLP 2023 Annual Conference.
Chin, H. “Psychiatric training in primary care medicine residency programs. A national survey”. Psychosomatics. Volume 41, Issue 5, September–October 2000, Pages 412-417. Kern, D, Thomas, P, Hughes, M. Curriculum Development for Medical Education: A Six-Step Approach, Second Edition. The Johns Hopkins University Press, 2009.
Discussion: While results of this needs assessment remain pending, it is anticipated that a statistically significant need related to anxiety and/or depressive disorder education will be discovered. There is also an anticipated interest in psychiatry clinical supervision to provide more psychiatric exposure. These results would likely bolster published evidence of the benefit of education and need of psychiatric didactic, however would provide more specific data on longitudinal curriculum implementation.
Conclusion: As access to timely psychiatric care remains limited, primary care physicians frequently become the only option to provide psychiatric care. Given the evidence of the need for more psychiatric education in primary care, the published benefit of brief psychiatric education, and discrepancy in required psychiatric education training volume compared to clinical practice, curriculum implementation within internal medicine residency programs remains essential to provide comfort in treatment and adequate care. While this study and anticipated results are limited by a small sample size and percentage of residents interested in primary care, the results of this needs assessment will provide the guideline for a longitudinal curriculum, of which will be implemented and then evaluated for its efficacy. The impact of a curriculum within one internal medicine program will assist in further study of curriculum use in other primary care specialties and ultimately education impact on patient care outcomes.
References:

