Training and Education
Session: Poster Session
(190) Lasting Impact of a Peer-to-Peer, Longitudinal Reproductive Psychiatry Curriculum for Obstetrics and Gynecology Residents: An Update on Resident Knowledge, Attitudes, and Comfort
Trainee Involvement: Yes

Isabella Kratzer, MD
Child & Adolescent Psychiatry Fellow
University of Pittsburgh Medical Center
Pittsburgh, Pennsylvania, United States.png)
Priya Gopalan, MD, FACLP (she/her/hers)
Associate Professor of Psychiatry
University of Pittsburgh Medical Center, Western Psychiatric Hospital
Pittsburgh, Pennsylvania, United States
Presenting Author(s)
Co-Author(s)
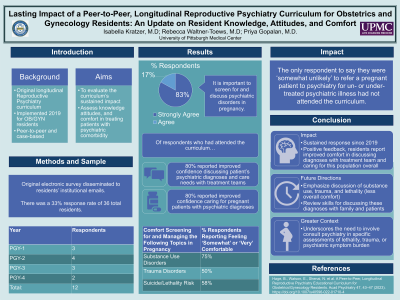
Background: Consultation-liaison psychiatrists are often at the forefront of providing psychiatric education to their non-psychiatric counterparts. Given the complexity of providing up-to-date, evidence-based care for pregnant patients with psychiatric conditions, an original, peer-to-peer, longitudinal reproductive psychiatry curriculum was implemented at our institution in 2019 for obstetrics and gynecology (OB/GYN) residents (Hage, 2022). In this needs assessment, we aimed to evaluate the sustained impact of this case-based curriculum on OB/GYN residents’ knowledge, attitudes, and comfort treating psychiatric populations, and their views on the curriculum four years after its implementation.
Methods: We disseminated an electronic survey over 3 weeks to 36 current OB/GYN residents at our institution, providing in-person and email reminders.
Hage, B., Watson, E., Shenai, N. et al. A Peer-to-Peer, Longitudinal Reproductive Psychiatry Educational Curriculum for Obstetrics/Gynecology Residents. Acad Psychiatry 47, 43–47 (2023). https://doi.org/10.1007/s40596-022-01710-4 Garbarino, A.H., Kohn, J.R., Coverdale, J.H. et al. Current Trends in Psychiatric Education Among Obstetrics and Gynecology Residency Programs. Acad Psychiatry 43, 294–299 (2019). https://doi.org/10.1007/s40596-019-01018-w
Results: Survey results were analyzed (n=12); 83% of respondents reported attending ‘some’ or ‘all’ of the longitudinal psychiatry sessions. All respondents ‘agreed’ or ‘strongly agreed’ that it is both their responsibility and important to screen for and discuss psychiatric disorders in pregnancy. Excluding data from the two respondents who reported attending none of the curriculum, 80% of remaining respondents said the curriculum improved their confidence in caring for pregnant patients with psychiatric diagnoses. Although 80% of respondents who had attended sessions reported improved confidence discussing patients’ psychiatric diagnoses and care needs with treatment teams, only 60% of responding attendees reported improved confidence discussing these issues with patients and families. While most respondents reported feeling ‘somewhat comfortable’ or ‘very comfortable’ counseling patients on substance use disorders (75%), medication management in pregnancy (75%), and outpatient mental health referrals (83%), fewer respondents reported similar comfort in assessing for trauma (50%) and lethality (58%). The only respondent to say they were ‘somewhat unlikely’ to refer a pregnant patient to psychiatry for un- or under-treated psychiatric illness had not attended the curriculum.
Discussion: All our respondents agreed or strongly agreed that screening for and discussing psychiatric disorders in pregnancy is both important and their responsibility, indicating a sustained response since the curriculum was initially implemented. Though most respondents reported improved confidence in caring for patients with psychiatric diagnoses following this longitudinal reproductive psychiatry curriculum, residents still reported lower levels of comfort addressing potentially stigmatized topics, such as discussing psychiatric diagnoses with patients and families or screening for trauma disorders and lethality.
Conclusion: These findings reinforce the utility of such curricula in improving OB/GYN residents’ comfort with caring for psychiatric patient populations, while underscoring the need to involve consult psychiatry in specific assessments of lethality, trauma, or psychiatric symptom burden. These data also suggest possible directions for curricular improvement, such as placing further emphasis on screening for trauma and lethality, effective communication about these diagnoses with patients and family, or assessment of the possible role of cultural stigma in residents’ comfort with these topics.
References:

