Psychopharmacology and Toxicology
Session: Poster Session
(144) Pathologic Skin Picking Resulting in Successive Bilateral Transmetatarsal Amputation
Trainee Involvement: Yes
- MS
Morgan Schmidt, MD (she/her/hers)
Resident Psychiatrist
Naval Medical Center San Diego
Poway, California, United States 
Amanda Ries, MD
Associate Program Director
Naval Medical Center San Diego
San Diego, California, United States
Presenting Author(s)
Co-Author(s)
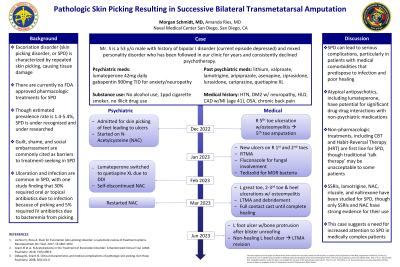
Background/Significance: While excoriation disorder has garnered increase attention since its inclusion in the DSM 5, there remains a paucity of data on the resultant medical complications. We present a case of a medically complicated patient with extensive psychiatric history, who developed osteomyelitis requiring multiple medical admissions and surgeries due to chronic skin picking. This case illustrates several points that consult-liaison psychiatrists should be aware of. First, excoriation disorder has the potential for severe medical complications, particularly in patients with medical comorbidities that predispose to infection and poor healing. Second, in multidrug resistant infections, there is potential for significant interactions with second generation antipsychotics, including the newest of its class, lumateperone. Third, treatment options for excoriation disorder with underlying bipolar illness are limited, but can include NAC and naltrexone. Lochner C, Roos A, Stein DJ. Excoriation (skin-picking) disorder: a systematic review of treatment options. Neuropsychiatr Dis Treat. 2017; 13:1867-1872 Grant JE et al. N-Acetylcysteine in the Treatment of Excoriation Disorder: A Randomized Clinical Trial. JAMA Psychiatry. 2016; 73(5):490-6 Odlaug BL, Grant JE. Clinical characteristics and medical complications of pathologic skin picking. Gen Hosp Psychiatry. 2008; 30(1):61-6
Case:
A 53-year-old male with history of bipolar I disorder, excoriation disorder with toenail picking, and other specified personality disorder and medical comorbidities of poorly controlled diabetes mellitus, CAD, and hypertension. He was followed in the outpatient clinic for years and was recently switched to lumateperone due to failure of numerous antipsychotics and mood stabilizers. He presented to the emergency department with right small toe discoloration after falling at home. He had a prior right small toe ulcer which his wife reported he had been picking. Exam showed gangrene and a large, full thickness ulcer. MRI showed osteomyelitis in the right fifth toe. He was admitted for IV antibiotics and underwent right fifth toe and metatarsal head amputation and debridement for source control. Surgical pathology showed growth of MSSA and enterococcus at the proximal margin and he was discharged on high dose oral Augmentin with a portable home wound vac. At his two-week follow-up with the limb salvage clinic, he had developed two new full-thickness ulcers on his right great and second toe as well as multiple, bilateral distal excoriations. He underwent a right transmetatarsal amputation (TMA) for source control and was placed in a total contact cast to limit skin picking. Post-operative tissue grew MRSA and VRE. He was discharged on oral Tedizolid after declining outpatient IV antibiotics, which required switching lumateperone to quetiapine, and he was recommended to start oral N-acetylcysteine (NAC) for compulsive skin picking. One month after the right TMA, he presented to the emergency room with wounds on his left great, second, and third toes with bone exposure as well as bilateral heel wounds. His wife reported he had continued to pick his feet. He required left TMA, which he underwent without complication. He was discharged to a SNF with both amputation sites healing well one-month post-hospitalization.
Discussion:
References:

