Child and Adolescent Psychiatry
Session: Poster Session
(038) Psychiatric Manifestations of Autoimmune Polyendocrine Syndrome in Adolescence: A Case Report
Trainee Involvement: Yes

Michelle Linke Shafa, MD
Child and Adolescent Psychiatry Fellow
Mayo Clinic
Rochester, Minnesota, United States
Sandra Rackley, MD, FACLP
CAP ED/CL Director
Mayo Clinic
Rochester, Minnesota, United States
Presenting Author(s)
Co-Author(s)
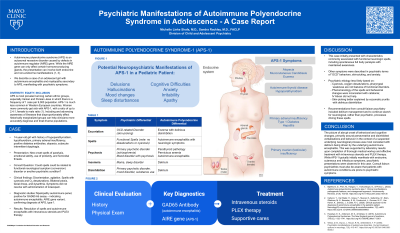
Introduction: Autoimmune polyendocrine syndrome, type 1 (APS-1) is an autosomal recessive disorder caused by defects in autoimmune regulator (AIRE) gene. While the AIRE gene can only affect certain hormone-producing glands, the presentation can involve both endocrine and non-endocrine manifestations (1, 2). We describe a case of an adolescent girl with autoimmune encephalitis and myelopathy secondary to APS-1, manifesting with psychiatric symptoms of excoriation, purposeless repetitive behaviors, and spells of full body paralysis. Clinicians need to be aware of this rare genetic condition in connection with autoimmune encephalitis when considering potential etiologies for spells. During a typical spell, the patient was reported to lose muscle tone and become unresponsive seconds to minutes. With this, there was a marked change from baseline behaviors, including increased emotional lability, use of profanity, and homicidal threats. Exam was significant for bilateral ptosis, facial droop, and dysarthria. Spells were at times also associated with cyanosis and oxygen desaturations. Her symptoms did not resolve with administration of lorazepam. Significant laboratory findings included the myelopathy autoimmune panel, positive for GAD65 Ab assay – indicating autoimmune encephalitis. Later studies revealed the AIRE gene variant, confirming diagnosis of APS-1. With intravenous steroids and PLEX therapy, autoimmune encephalitis and spells resolved. While functional neurological spell (conversion) is reasonable to have on a thorough differential diagnosis, oxygen desaturation and pharyngeal weakness are not a feature of conversion disorders. The phenomenology of the spells and behavioral changes were inconsistent with catatonia; IV Ativan did not help. Recommendations from consult-liaison psychiatry included delirium management and to continue search for neurological, rather than psychiatric, processes driving these spells. Bjørklund, G., Pivin, M., Hangan, T., Yurkovskaya, O., & Pivina, L. (2022). Autoimmune polyendocrine syndrome type 1: Clinical manifestations, pathogenetic features, and management approach. Autoimmunity Reviews, 21(8), 103135. https://doi.org/10.1016/j.autrev.2022.103135 Husebye, E. S., Anderson, M. S., & Kämpe, O. (2018). Autoimmune Polyendocrine Syndromes. The New England journal of medicine, 378(12), 1132–1141. https://doi.org/10.1056/NEJMra1713301
Case: A 14-year-old girl with history of hypoparathyroidism, hypothyroidism, primary adrenal insufficiency, positive diabetes antibodies, alopecia, subacute intermittent dysphagia presented with new onset spells of paralysis and paresthesia. Psychiatry was asked to comment on whether the spells could be related to functional neurological symptom (conversion) disorder or another psychiatric condition.
Discussion: This case initially presented with characteristics commonly associated with functional neurologic spells, including spontaneous full body paralysis with maintained awareness. Other symptoms were described in psychiatric terms of “OCD” behaviors, skin-picking, and anxiety. The most commonly non-endocrine presenting symptoms of APS-1 are cutaneous and infectious (1) and not psychiatric.
Conclusion: The picture of abrupt onset of behavioral and cognitive changes, primarily around perseverative and disinhibited verbalizations and behavior in the context of a suspected underlying neurological process was most consistent with delirium being driven by the underlying autoimmune encephalitis. This was supported by laboratory results upon completion of thorough medical workup and effective treatment with intravenous steroids and PLEX therapy. While APS-1 typically initially manifests with endocrine, cutaneous and infectious symptoms, psychiatric presentations were observed in this case.
References:

