Catatonia
Session: Poster Session
(028) Recurring Catatonia: Diagnostic Challenges and Clinical Significance
Trainee Involvement: No
- YM
Yara Moustafa, MD. PhD.
Senior Associate Consultant
Mayo Clinic
Jacksnville, Florida, United States - TR
Teresa Rummans, FACLP
Professor of Psychiatry
Mayo Clinic
Rochester, Minnesota, United States - AV
Adriana Vasquez, M.D., FAPA, FACLP
Consultant Psychiatry. Chair of Psychiatry and Psychology Specialty Council Transplant.
Mayo Clinic
Jacksonville, Florida, United States 
Barbara Lubrano di Ciccone, MD, FACLP
Senior Associate Consultant
Mayo Clinic
Jacksonville, Florida, United States
Presenting Author(s)
Co-Author(s)
Introduction Case Presentation Discussion References 1. Walther S, Strik W. Catatonia. CNS Spectr. 2016;21(4):341-8. 2. Carroll BT. Catatonia: A Clinician's Guide to Diagnosis and Treatment. By M. Fink and M. A. Taylor. (Pp. 256; Price $50.00, ISBN 0-521-82226-2 hb.) Cambridge University Press: Cambridge, UK. 2003. Psychological Medicine. 2004;34(6):1139-40. 3. Joan Roig Llesuy, M.D., Michel Medina, M.D., Kristen C. Jacobson, Ph.D., Joseph J. Cooper, M.D. Catatonia Under-Diagnosis in the General Hospital. The Journal of Neuropsychiatry and Clinical Neurosciences. 2018;30(2):145-51. 4. Walther S, Stegmayer K, Wilson JE, Heckers S. Structure and neural mechanisms of catatonia. Lancet Psychiatry. 2019;6(7):610-9. 5. Biles TR, Anem G, Youssef NA. Should Catatonia Be Conceptualized as a Pathological Response to Trauma? The Journal of Nervous and Mental Disease. 2021;209(5):320-3.
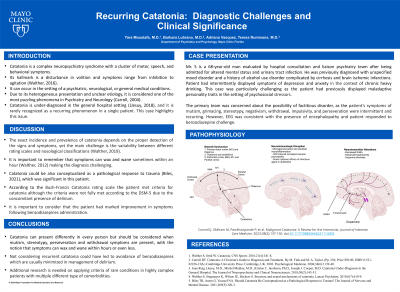
Catatonia is a complex neuropsychiatry syndrome with a cluster of motor, speech, and behavioral symptoms. Its Hallmark is a disturbance in volition and symptoms range from inhibition to agitation (Walther, 2016). It can occur in the setting of a psychiatric, neurological, or general medical condition. Due to its heterogeneous presentation and unclear etiology, it is considered one of the most puzzling phenomena in Psychiatry and Neurology (Carroll, 2004). Catatonia is under-diagnosed in the general hospital setting (Llesuy, 2018), and it is rarely recognized as a recurring phenomenon in a single patient. This case highlights this issue.
Mr. S is a 68-year-old man evaluated by hospital psychiatry team after being admitted for altered mental status and urinary tract infection. He was previously diagnosed with unspecified mood disorder and a history of alcohol use disorder complicated by cirrhosis and brain ischemic infarctions. Patient had intermittently displayed symptoms of depression and anxiety in the context of chronic heavy drinking. This case was particularly challenging as the patient had previously displayed maladaptive personality traits in the setting of psychosocial stressors. The primary team was concerned about the possibility of factitious disorder, as the patient’s symptoms of mutism, grimacing, stereotypy, negativism, withdrawal, impulsivity, and perseveration were intermittent and recurring. However, EEG was consistent with the presence of encephalopathy and patient responded to benzodiazepine challenge.
The exact incidence and prevalence of catatonia depends on the proper detection of the signs and symptoms, yet the main challenge is the variability between different rating scales and nosological classifications (Walther, 2019). It is important to remember that symptoms can wax and wane sometimes within an hour (Walther, 2012) making the diagnosis challenging. Catatonia could be also conceptualized as a pathological response to trauma (Biles, 2021), which was significant in this patient. According to the Bush-Francis Catatonia rating scale the patient met criteria for catatonia although the criteria were not fully met according to the DSM-5 due to the concomitant presence of delirium. It is important to consider that the patient had marked improvement in symptoms following benzodiazepines administration. Not considering recurrent catatonia could have led to avoidance of benzodiazepines which are usually minimized in management of delirium. Additional research is needed on applying criteria of rare conditions in highly complex patients with multiple different type of comorbidities.

