Neurocognitive Disorders, Delirium, and Neuropsychiatry
Session: Poster Session
(111) Risk Factors and Progression of Subsyndromal Delirium in Older Patients With Hip Fracture Surgery
Trainee Involvement: No

Yanin Thipakorn, MD
Psychiatrist
King Chulalongkorn Memorial Hospital, Krung Thep, Thailand- PT
Paul Thisayakorn, MD
Assistant Professor
Department of Psychiatry, Faculty of Medicine, Chulalongkorn University
Bangkok, Krung Thep, Thailand - ST
Saran Tantavisut, MD, PhD
Associate Professor
Department of orthopedics, Faculty of Medicine, Chulalongkorn University
Bangkok, Krung Thep, Thailand - KW
Krittin Wannarong, Bachelor of medicine
Psychiatric resident
Department of psychiatry, Faculty of medicine, Chulalongkorn university, Bangkok, Thailand
Muang district, Samut Prakan, Thailand - ps
patchara suttayakom, n/a
Medical student
Faculty of Medicine, Chulalongkorn University
bangkok, Krung Thep, Thailand
Presenting Author(s)
Co-Author(s)
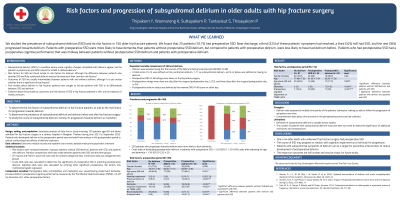
Background: Subsyndromal delirium (SSD) is a condition where acute cognitive changes compatible with delirium appear, but the patient’s symptoms do not fulfill criteria for a DSM-5-defined delirium. Outcomes of patients with SSD are generally intermediate between patients with and without delirium and may be a group of patients where management is warranted. There have been no studies on SSD in the geriatric hip fracture population. We aimed to assess the incidence and prevalence of SSD, characterize the risk factors of perioperative SSD in older patients with hip fractures, its impact on patient outcomes, and the course of SSD. Methods: This was a secondary analysis of a cross-sectional study involving patients aged 65 and above admitted for hip fracture surgery (IRB no. 564/63). Delirium was assessed using the DRS-R-98 before the surgery and postoperative days two and four. Risk factors and postoperative complications were collected by patient and family interview and chart review. Descriptive statistics were used to compare presence of risk factors and complications between patients without SSD/delirium, patients with SSD, and patients with delirium in the preoperative and postoperative period. Results: For the preoperative period, we analyzed data from 150 patients. The prevalence of preoperative SSD and delirium was 16.7% and 24% respectively. The prevalence increased to 18.7% and 36% after surgery. The incidence of postoperative-onset SSD and delirium was 15.7% and 19.3%. The risk factor that was more prevalent in patients with preoperative SSD compared to patients without preoperative SSD/delirium was dementia (32% VS 3.4%, p< 0.001). The risk factor that differentiated preoperative SSD from delirium was having a previous episode of delirium (12% VS 36.1%, p<span lang="TH">=0.035). For postoperative SSD and postoperative delirium, the risk factor that had significantly different prevalence was dementia (8% VS 36.4%, p<span lang="TH">=0.030). Sepsis was more common in patients with postoperative SSD compared to patients without SSD/delirium. Near discharge, patients who had preoperative SSD had resolved symptoms, had SSD, or developed delirium in equal proportions (32% VS 32% VS 36%). Discussion: In older patients with hip fractures, SSD is more likely to occur during the preoperative period, and may resolve, continue, or progress. Dementia on admission is a risk factor for both SSD and delirium but is more common in patients with delirium. The age and cognitive performance of patients with SSD tend to be intermediate between patients with and without delirium. Impact on outcomes is still unclear and should be further studied. Conclusion: Around one in six older adults who underwent hip fracture surgery had perioperative SSD. Patients with SSD may represent an intermediate stage from which patients may develop delirium. Interventions at this stage may help prevent delirium in patients with hip fractures.
References:
Meagher D, O’Regan N, Ryan D et al. Frequency of delirium and subsyndromal delirium in an adult acute hospital population. BJPsych 2014; 205: 478-485.
Serafim RB, Dal-Pizzol F, Souza-Dantas V et al. Impact of Subsyndromal Delirium Occurrence and Its Trajectory during ICU Stay. J Clin Med 2022; 11: 6797.

