Catatonia
Session: Poster Session
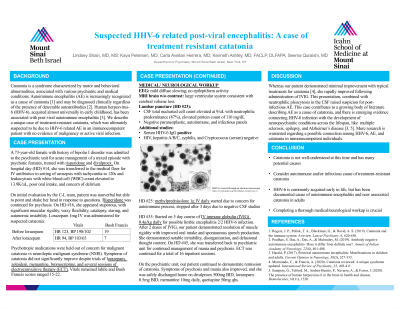
(021) Suspected HHV-6 Related Post-viral Encephalitis: A Case of Treatment Resistant Catatonia
Trainee Involvement: Yes

Lindsey Shain, MD
Psychiatry Resident
Mount Sinai Beth Israel
New York, New York, United States- KP
Kaya Petersen, MD
Psychiatry Resident
Mount Sinai Beth Israel
New York, New York, United States - CA
Carla Avellan Herrera, MD
Consultation Liaison Fellow
Mount Sinai Beth Israel
New York, New York, United States 
Kenneth Ashley, MD, FACLP, DLFAPA
Associate Professor
Mount Sinai Beth Israel
New York, New York, United States- SQ
Seema Quraishi, MD
Division Chief and Fellowship Program Director, Consultation-Liaison Psychiatry
Mount Sinai Beth Israel
Astoria, New York, United States
Presenting Author(s)
Co-Author(s)
Catatonia is a syndrome characterized by motor and behavioral abnormalities, associated with various psychiatric and medical conditions. Autoimmune encephalitis (AE) is increasingly recognized as a cause of catatonia (Rogers et al., 2019), and may be diagnosed clinically regardless of the presence of detectable autoantibodies (Pradhan et al., 2019). Human herpesvirus-6 (HHV-6), acquired almost universally in early childhood, has been associated with post-viral autoimmune encephalitis (Harald, 2017). We describe a unique case of treatment-resistant catatonia, which was ultimately suspected to be due to HHV-6 related AE in an immunocompetent patient with no evidence of malignancy or active viral infection. A 73-year-old woman with a history of bipolar I disorder was admitted to the psychiatric unit for acute management of a mixed episode with psychotic features. She was later transferred to the medical floor for IV antibiotics in the setting of urinary tract infection, poor oral intake, and concerns of delirium. On initial assessment by the consult psychiatry team, the patient appeared grossly psychotic and was restarted on risperidone. The following day, she developed symptoms concerning for malignant catatonia versus neuroleptic malignant syndrome. Risperidone was discontinued, and the patient did not improve despite trials of lorazepam, zolpidem, memantine, bromocriptine, and several sessions of electroconvulsive therapy (ECT). Extensive neurological and medical workup was performed. EEG revealed mild diffuse slowing. Lumbar puncture (LP) was remarkable only for WBC count of 9/uL and neutrophilic predominance (87%), elevated protein count of 116 mg/dL. Infectious and autoimmune workup was significant only for positive serum HHV-6 IgG; serum anti-NMDA receptor antibodies were negative. IV methylprednisolone was trialed and discontinued due to lack of response. Patient finally responded dramatically to IVIG. Whereas our patient demonstrated minimal improvement with typical treatments for catatonia (Mormando & Francis, 2020), she rapidly improved following administration of IVIG. This presentation, combined with neurological workup demonstrating CSF with neutrophilic pleocytosis raises suspicion for post-infectious AE. This case contributes to a growing body of literature describing AE as a cause of catatonia, and there is emerging evidence connecting HHV-6 infection with the development of neuropsychiatric conditions across the lifespan, like multiple sclerosis, epilepsy, and Alzheimer’s disease (Harald, 2017; Santpere, 2020). More research is warranted regarding a possible connection among HHV-6, AE, and catatonia in immunocompetent individuals.
Background:
Case:
Discussion:
References:
Harald, P. (2017). Postviral autoimmune encephalitis: Manifestations in children and adults. Current Opinion in Neurology, 30(3), 327-333.
Mormando, C., & Francis, A. (2020). Catatonia reviewed: A unique syndrome updated. International Review of Psychiatry, 32, 403-411.
Pradhan, S. Das, A., Das, A., & Mulmuley, M. (2019). Antibody negative autoimmune encephalitis- Does it differ from definite one? Annals of Indian Academy of Neurology, 22(4), 401-408.
Rogers, J. P., Pollak, T. A., Blackman, G., & David, A. S. (2019). Catatonia and the immune system: A review. Lancet Psychiatry, 6, 620-630.
Santpere, G., Telford, M., Andres-Benito, P., Navarro, A., & Ferrer, I. (2020). The presence of human herpesvirus 6 in the brain in health and disease. Biomolecules, 10(11), 1520.

