Catatonia
Session: Poster Session
(018) The Impact of a National Injectable Lorazepam Shortage on the Treatment of Catatonia in the General Hospital
Trainee Involvement: Yes
.jpeg.jpg)
Kenneth Novoa, MD, FACLP (he/him/his)
Medical Director - Consultation-Liaison Psychiatry Service
Denver Health Medical Center
Denver, Colorado, United States
Thida Thant, MD
Assistant Professor of Psychiatry
University of Colorado School of Medicine
Aurora, Colorado, United States
Daniel J. Grine, MD
Resident Psychiatrist
HCA HealthONE
Loveland, Colorado, United States- AE
Annette Encinias, MS Information Technology
Data Team Admiinstrator
Denver Health and Hospital Authority
Arvada, Colorado, United States 
Merlin Ariefdjohan, PhD, MPH
Assistant Professor
Department of Psychiatry, University of Colorado Anschutz Medical Campus
Aurora, Colorado, United States
Presenting Author(s)
Co-Author(s)
Background/Significance Fink M, Bush G, Francis A: Catatonia: a treatable disorder, occasionally recognized, Direct Psychiatry 13:1-7, 1993.
For many years, lorazepam has been considered a first-line treatment for catatonia (Rosebush, 1990). Due to a less rapid and less extensive drug distribution that can maintain relatively high plasma levels, intravenous lorazepam is usually the preferred formulation (Fink, 1993). Given the recent and on-going national shortage of injectable (intravenous and intramuscular) lorazepam (FDA, 2023), we are investigating the clinical impact this is having on our patients with catatonia.
Methods
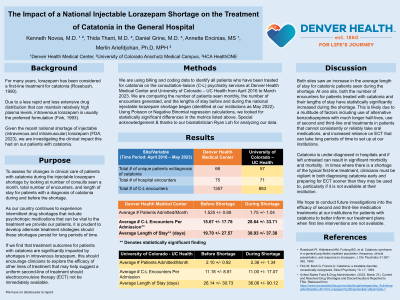
We are using billing and coding data to identify all patients who have been treated for catatonia on the consultation-liaison psychiatry services at two affiliated hospitals from April 2016 to March 2023. Using this data, we are comparing the number of patients seen monthly, the lengths of stay, and the number of encounters generated before and after the national lorazepam shortage began (identified at our institutions as May 2022).
Results
We are still collecting data at the time of this submission. We fully expect to have complete and meaningful data in time for the conference. Thus far, at one institution, the average and median lengths of stay for patients treated for catatonia prior to the lorazepam shortage was 22 and 13 days, respectively. The average and median lengths of stay for patients treated for catatonia during the lorazepam shortage was 39 and 27 days, respectively. The average and median number of new patients seen monthly for treatment of catatonia prior to the shortage was 0.6 and 0, respectively. The average and median number of new patients seen monthly for treatment of catatonia during the shortage was 1.1 and 1, respectively.
Discussion
As we anticipated, both the number of patients seen monthly for treatment of catatonia and their lengths of stay have increased during the lorazepam shortage period. This is likely due to a multitude of factors: use of alternative benzodiazepines with much longer half-lives, use of second and third-line oral treatments in patients that cannot consistently or reliably take oral medications, and increased reliance on electroconvulsive therapy (ECT) that can take long periods of time to set up at our institutions.
Conclusion/Implications
Catatonia is under-diagnosed in hospitals and if left untreated can result in significant morbidity and mortality. In times where there is a shortage of the typical first-line treatment, clinicians must be vigilant in both diagnosing catatonia early and preparing for ECT sooner than they may be used to, particularly if it is not available at their institution.
References
Rosebush PI, Hildebrand AM, Furlong BG, et al: Catatonic syndrome in a general psychiatric inpatient population: frequency, clinical presentation, and response to lorazepam, J Clin Psychiatry 51:357-362, 1990.
United States Food & Drug Administration. (2023, March 31). Current and Resolved Drug Shortages and Discontinuations Reported to FDA. Retrieved from https://www.accessdata.fda.gov/scripts/drugshortages/dsp_ActiveIngredientDetails.cfm?AI=Lorazepam%20Injection&st=c&tab=tabs-1

