Transplant Psychiatry
Session: Poster Session
(204) The Rochester Relapse Risk Scale: Farther Along the Path to a Standardized Approach to Predicting Substance Relapse in Liver Transplant Candidates
Trainee Involvement: Yes

Tara Cicic, BA (she/her/hers)
Medical Student
University of Rochester School of Medicine
Rochester, New York, United States- JM
John Martens, MPH
Data and Quality Administrator
University of Rochester Medical Center Transplant Institute
Rochester, New York, United States 
Mark Nickels, MD
Director, Transplant Psychiatry
University of Rochester Medical Center, Dept. of Psychiatry
Rochester, New York, United States
Presenting Author(s)
Co-Author(s)
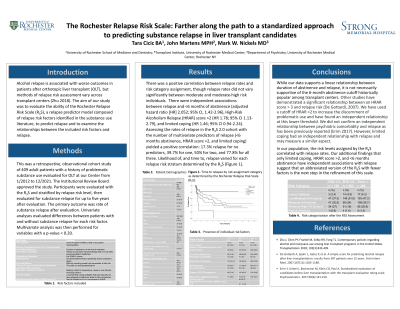
Background Alcohol relapse is associated with worse outcomes in patients after orthotopic liver transplant (OLT) but methods of relapse risk assessment vary across transplant centers (Zhu 2018). The aim of our study was to evaluate the ability of the Rochester Relapse Risk Scale (R3S), a relapse predictor model composed of relapse risk factors identified in the substance use literature, to predict relapse and to examine the relationships between the included risk factors and relapse. Methods This was a retrospective, observational cohort study of 409 adult patients with a history of problematic substance use evaluated for OLT at our Center from 1/2012 to 12/2021. The Institutional Review Board approved the study. Participants were evaluated with the R3S and stratified by relapse risk level, then evaluated for substance relapse for up to five years after evaluation. The primary outcome was rate of substance relapse after evaluation. Univariate analyses evaluated differences between patients with and without substance relapse for each risk factor. Multivariate analysis was then performed for variables with a p-value < 0.20. Results There was a positive correlation between relapse rates and risk category assignment, though relapse rates did not vary significantly between moderate and moderate-high risk individuals. There were independent associations between relapse and < 6 months of abstinence (adjusted hazard ratio [HR] 2.052; 95% CI, 1.42-2.96), High-Risk Alcoholism Relapse (HRAR) score >2 (HR 1.78; 95% CI 1.13-2.79), and limited coping (HR 1.46; 95% CI 0.94-2.24). Discussion While our data supports a linear relationship between duration of abstinence and relapse, it is not necessarily supportive of the 6-month abstinence cutoff historically popular among transplant centers. Other studies have demonstrated a significant relationship between an HRAR score > 3 and relapse risk (De Gottardi, 2007). We have used a cutoff of HRAR >2 to increase the discernment of problematic use and have found an independent relationship at this lower threshold. We did not confirm an independent relationship between psychiatric comorbidity and relapse as has been previously reported (Erim 2017). However, limited coping had an independent relationship with relapse and may measure a similar aspect. Conclusion In our population, the risk levels assigned by the R3S correlated with relapse rates. Our additional findings that only limited coping, HRAR score >2, and < 6 months abstinence have independent associations with relapse suggest that an abbreviated version of the R3S with fewer factors is the next step in the refinement of this scale. References De Gottardi A, Spahr L, Gelez P, et al. A simple score for predicting alcohol relapse after liver transplantation: results from 387 patients over 15 years. Arch Intern Med. 2007;167(11):1183-1188. Erim Y, Scheel J, Beckmann M, Klein CG, Paul A. Standardized evaluation of candidates before liver transplantation with the transplant evaluation rating scale. Psychosomatics. 2017;58(2):141-150. Zhu J, Chen PY, Frankel M, Selby RR, Fong TL. Contemporary policies regarding alcohol and marijuana use among liver transplant programs in the United States. Transplantation 2018; 102(3):433-439.

