Quality and Safety
Session: Poster Session
(168) Trauma-Informed Approach to Psychiatric Sequelae of Firearm Injuries: A Case Report and Literature Review
Trainee Involvement: Yes

Sanjana Kumar, MD (she/her/hers)
PGY-3 Psychiatry Resident
UMass Chan Medical School - Baystate Medical Center
Springfield, Massachusetts, United States
Deepika Sundararaj, MD
Consultation-Liaison Psychiatry
UMass Chan Medical School - Baystate Medical Center
Bloomfield, Connecticut, United States
Presenting Author(s)
Co-Author(s)
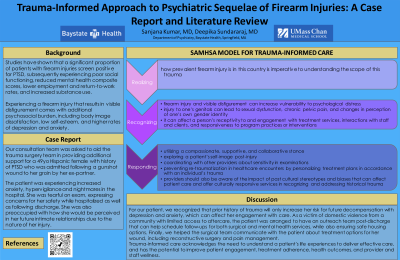
Background/Significance: Studies have shown that a significant proportion of patients with firearm injuries screen positive for PTSD experiencing poor social functioning, reduced mental health composite scores, lower employment and return-to-work rates, and increased substance use. A firearm injury that results in visible disfigurement comes with additional psychosocial burden. Methods/ Realizing how prevalent firearm injury is in this country is imperative to understanding the scope of this trauma. Recognizing that firearm injury and visible disfigurement can increase vulnerability to psychological distress. Furthermore, injury to one’s genitals can lead to sexual dysfunction, chronic pelvic pain, and changes in perception of one’s own gender identity. Treatment-wise, it can affect a person’s receptivity to and engagement with treatment services and responsiveness to program practices or interventions. Responding by using the above knowledge to inform one’s care of the patient. This could involve utilizing a compassionate, supportive, and collaborative stance; exploring a patient’s self-image post-injury; coordinating with other providers about sensitivity in examinations; and preventing retraumatization in healthcare encounters by personalizing treatment plans in accordance with an individual’s trauma. It is vital for providers to be aware of the impact of past cultural stereotypes and biases that can affect patient care. Providers need to offer culturally responsive services when recognizing and addressing historical trauma. References Sarwer DB, Siminoff LA, Gardiner HM, Spitzer JC. The psychosocial burden of visible disfigurement following traumatic injury. Front Psychol. 2022 Aug 30;13:979574.
Case Presentation: Our consultation team was asked to aid the surgical team in providing additional support for a 49yo Hispanic female with history of PTSD who was admitted following a gunshot wound to her groin by her ex-partner. Patient was experiencing increased anxiety, hypervigilance and nightmares in the hospital. Patient was tearful on exam expressing concerns for her safety as well as preoccupation with how she would be perceived in her future relationships due to the nature of her injury.
Results: In creating our treatment plan for our patient, we reviewed the many trauma-informed care models before identifying the SAMHSA model for trauma-informed approach:
Discussion: For our patient, we recognized that prior history of trauma will only increase her risk for future decompensation with depression and anxiety which can affect her engagement with care. As a victim of domestic violence from a community with limited access to aftercare, patient was arranged to have an outreach team post-discharge that can help schedule follow up for both surgical and mental health services while also ensuring safe housing options. Finally, we helped surgical team communicate with patient about treatment options for her wound including reconstructive surgery and pain management.
Conclusion: Trauma-informed care acknowledges the need to understand a patient's life experiences in order to deliver effective care and has the potential to improve patient engagement, treatment adherence, health outcomes, and provider and staff wellness.
Center for Substance Abuse Treatment (US). Trauma-Informed Care in Behavioral Health Services. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 2014. (Treatment Improvement Protocol (TIP) Series, No. 57.) Chapter 1, Trauma-Informed Care: A Sociocultural Perspective.

