Child and Adolescent Psychiatry
Session: Poster Session
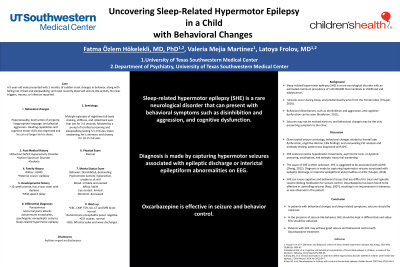
(034) Uncovering Sleep-Related Hypermotor Epilepsy in a Child with Behavioral Changes
Trainee Involvement: Yes

Fatma Ozlem Hokelekli, MD, PhD (she/her/hers)
Resident Physician
University of Texas Southwestern Medical Center
Dallas, Texas, United States- VM
Valeria Mejia Martinez, n/a
Medical Student
UT Southwestern
Dallas, Texas, United States - LF
Latoya Frolov, MD
Assistant Professor of Psychiatry
UT Southwestern Medical Center
Plano, Texas, United States
Presenting Author(s)
Co-Author(s)
Background
Sleep-related hypermotor epilepsy (SHE) is a rare neurological disorder with an estimated minimum prevalence of 1.8/100,000 that manifests in childhood and adolescence. Seizures occur during sleep, and predominantly arise from the frontal lobes (Tinuper, 2016). Behavioral disturbances, such as disinhibition and aggression, and cognitive dysfunction can be seen (Braakman, 2011). Seizures may not be noticed early on, and behavioral changes may be the only presenting symptom to the clinic. Case Discussion Conclusion In patients with behavioral changes and sleep-related symptoms, seizures should be ruled out. In the presence of seizure-like behavior, SHE should be kept in differentials and video-EEG should be obtained. Patients with SHE may achieve good seizure and behavioral control with Oxcarbazepine treatment.
A 9-year-old male presented with 5 months of sudden onset changes in behavior, along with falling out of bed and sleepwalking, and most recently observed seizure-like activity. No clear triggers, trauma, or infection reported.
Behavioral changes:
Hypersexuality, destruction of property, inappropriate language, and physical aggression. Reading capabilities and cognitive motor skills also regressed and he can no longer tie his shoes.
Seizure
Description:
Multiple episodes of nighttime full-body shaking, stiffness, and rolled back eyes that last for 3-4 seconds, followed by a period of terrified screaming and sleepwalking lasting 3-5 minutes. Upon awakening, he is amnestic and drowsy for 10-15 minutes.
PMH: Attention Deficit Hyperactivity Disorder (ADHD) and Autism Spectrum Disorder, both diagnosed after behavioral changes
Family History: father with ADHD and paternal cousin with epilepsy
Work up:
- CBC, CMP, TSH, UA, CT and MRI brain: normal.
- Autoimmune encephalitis panel: negative.
- CSF studies: normal
- EEG: bifrontal spike and wave discharges.
Differentials for this patient included parasomnias, nocturnal panic attacks, autoimmune encephalitis, psychogenic nonepileptic seizures, and SHE. Given typical seizure semiology, behavioral changes related to frontal lobe dysfunction, cognitive decline, EEG findings; and unrevealing CSF analysis and antibody testing, patient was diagnosed with SHE.
SHE seizures involve hyperkinetic movements, asymmetric tonic or dystonic posturing, vocalization, and epileptic nocturnal wandering. The cause of SHE is often unknown. SHE is suggested to be associated with ADHD (Zhang, 2012). Diagnosis is made by capturing hypermotor seizures associated with epileptic discharge or interictal epileptiform abnormalities on EEG (Tinuper, 2016).
SHE can cause cognitive and behavioral issues that are difficult to treat and typically require lifelong medication for seizure control. Oxcarbazepine has been found to be effective in controlling seizures (Raju, 2007), resulting in an improvement in behavior, as was observed in this patient.
References:
Tinuper P, et al. R. Definition and diagnostic criteria of sleep-related hypermotor epilepsy. Neurology. 2016 May 10;86(19):1834-42.
Braakman HM, et al. Cognitive and behavioral complications of frontal lobe epilepsy in children: a review of the literature.
Zhang DQ, et al. Clinical observations on attention-deficit hyperactivity disorder (ADHD) in children with frontal lobe epilepsy. J Child Neurol. 2014 Jan;29(1):54-7.
Raju GP, et al. Oxcarbazepine in children with nocturnal frontal-lobe epilepsy. Pediatr Neurol. 2007 Nov;37(5):345-9.

