Catatonia
Session: Poster Session
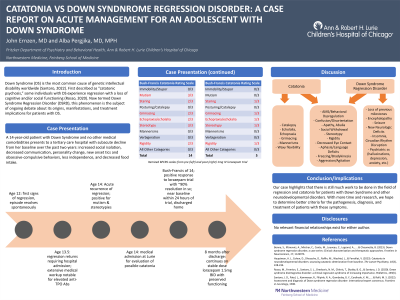
(016) Catatonia vs Down Syndrome Regression Disorder: A Case Report on Acute Management for an Adolescent with DS
Trainee Involvement: Yes
- JE
John Ernzen, MD (he/him/his)
Child & Adolescent Psychiatry Fellow
Ann & Robert H. Lurie Children's Hospital of Chicago
Chicago, Illinois, United States - AP
Alba Pergjika, MD
Medical Director, Psychiatry and Behavioral Health Consultation Liaison Service
Ann & Robert H. Lurie Children's Hospital of Chicago
Chicago, Illinois, United States
Presenting Author(s)
Co-Author(s)
Background/Significance:
Down Syndrome (DS) is the most common cause of genetic intellectual disability worldwide (Santoro, 2022). First described as “catatonic psychosis”, some individuals with DS experience regression with a loss of cognitive and/or social functioning (Rosso, 2020). Now termed Down Syndrome Regression Disorder (DSRD), this phenomenon is the subject of ongoing debate about its origins, manifestations, and implications for patients with DS. Case: A 14-year-old patient with Down Syndrome and no other medical comorbidities presents with subacute decline from her baseline over the past two years: increased social isolation, decreased communication, personality change, new onset tics and obsessive-compulsive behaviors, less independence, and decreased food intake. Three episodes of acute worsening occurred with catatonic-like symptoms with the last one resulting in minimal recovery. She returned to near baseline after receiving intranasal midazolam prior to a planned electroencephalogram as part of a thorough medical work up. There was an unrevealing lumbar puncture and normal brain imaging. The only significant laboratory finding was elevated anti-TPO antibodies, which endocrinology recommended following but not actively treating. Patient was admitted to the pediatric service at recommendation of her outpatient team for evaluation and management of possible catatonia. The psychiatry consult liaison service evaluated patient who scored 14 on the Bush-Francis Catatonia Rating Scale. Administration of Lorazepam IV 1mg reduced symptoms significantly with repeat BFCRS of 5. A repeat dose of lorazepam IV 0.5mg was given with resolution of symptoms. Patient was discharged home on oral lorazepam 1mg in the morning and 0.5mg at night. This case highlights our limited understanding of the overlap between catatonia and regression in patients with DS. Published case reports suggest that DSRD responds most to lorazepam and/or electroconvulsive therapy, with a subset of patients responding to immunotherapy as well. Persons with Down syndrome are known to have higher rates of catatonia, which is a common feature of regression. This patient’s positive response to lorazepam is suggestive of underlying catatonia possibly as a component of DSRD (Hauptman, 2023). Conclusion/Implications: There is still much work to be done in the field of regression and catatonia for patients with Down Syndrome and other neurodevelopmental disorders. With more time and research, we hope to determine better criteria for the pathogenesis, diagnosis, and treatment of patients with regression and/or catatonic symptoms. Hauptman, A. J., Cohen, D., Dhossche, D., Raffin, M., Wachtel, L., & Ferrafiat, V. (2023). Catatonia in neurodevelopmental disorders: assessing catatonic deterioration from baseline. The Lancet Psychiatry, 10(3), 228-234. Rosso, M., Fremion, E., Santoro, S. L., Oreskovic, N. M., Chitnis, T., Skotko, B. G., & Santoro, J. D. (2020). Down syndrome disintegrative disorder: a clinical regression syndrome of increasing importance. Pediatrics, 145(6). Santoro, J. D., Patel, L., Kammeyer, R., Filipink, R. A., Gombolay, G. Y., Cardinale, K. M., ... & Rafii, M. S. (2022). Assessment and diagnosis of Down syndrome regression disorder: international expert consensus. Frontiers in neurology, 1508.
Discussion:
References:

