Diversity, Equity, and Inclusion
Session: Poster Session
(076) The Menopause and Minority Health Project: An Innovative and Interdisciplinary Education Project
Trainee Involvement: No

Sarah Nagle-Yang, MD
Associate Professor of Psychiatry
University of Colorado School of Medicine
Denver, Colorado, United States- PP
Phoutdavone Phimphasone-Brady, PhD
Assistant Professor
University of Colorado Anschutz Medical Campus
Aurora, Colorado, United States 
Laura Borgelt, PharmD, FCCP
Professor and Associate Vice Chancellor of Strategic Initiatives
University of Colorado Anschutz Medical Campus
Aurora, Colorado, United States- NS
Nanette Santoro, MD
Professor and Chair of Ob-Gyn
University of Colorado school of Medicine
Aurora, Colorado, United States 
Helen L. Coons, PhD
Associate Professor & Clinical Director, Women's Behavioral Health & Wellness Programs, Psychiatry
University of Colorado School of Medicine
Denver, Colorado, United States
Presenting Author(s)
Co-Author(s)
Background/Significance: The past three decades have seen substantial advances in the understanding of menopause, including increased recognition of the strong influence of race and ethnicity. Unfortunately, the education of clinicians has lagged, resulting in primary care, psychiatry and ob/gyn physicians who do not feel confident in menopause care. Evidence suggests that those who seek care for menopause-related concerns experience significant racial and ethnic disparities, including the degree women are thoroughly evaluated for menopausal symptoms and their impact on functioning or quality of life, and likelihood of discussing or prescribing menopausal hormone replacement therapy when indicated. Given the boundary spanning roles common in consult liaison (CL) psychiatry, CL psychiatrists are well positioned to engage in interdisciplinary education around the best practices in menopause care. Conclusion/Implications: The ECHO Colorado learning approach combined with the innovative XR simulations resulted in positive improvements in provider knowledge, confidence, and treatment of racial and ethnic differences in menopause care.
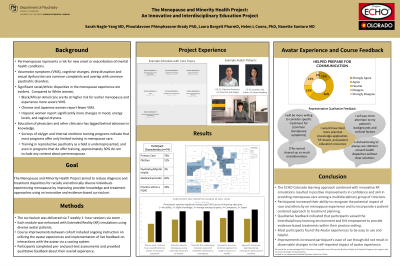
Methods: The Departments of Psychiatry, Obstetrics and Gynecology, and the School of Pharmacy partnered with the Extension of Community Health Outcomes (ECHO) Colorado, an online network that provides education to community providers about the management of complex medical conditions in underserved populations. The proven ECHO collaborative learning approach was enhanced with Extended Reality (XR) simulations using diverse avatar ‘patients’ with emotional responses and compounded interactions to engage a deeper understanding of menopause experiences in minority women. Seven evidence-based modules were presented, covering the topics of: 1) intersectionality, 2) vasomotor symptoms, 3) mood and anxiety, 4) sleep, 5) bleeding and hysterectomy, 6) weight, body image, and sexual health, and 7) menopause-related treatment. Most participants were either primary care or ob-gyn clinicians. Participants completed brief pre and posttest assessments prior to each session and completed the avatar experiences. Descriptive statistics are provided. This study was considered exempt research by the Colorado Multiple IRB.
Results: Seventy-four participants participated in the series within 3 discrete cohorts. Most (86%) participants practiced within an urban setting, though the series included participants from rural (13%) and frontier (1%) areas of Colorado as well. Eighty-seven percent of participants reported caring for patients who are insured by Medicaid, and half (51%) reported that their practice primarily provided care to an underserved population. Participant’s self-reported skill level after completing the series was increased (p < 0.001) across all learning objectives. Most (79%) felt that the avatars were easy to use, and 61% felt that they helped prepare the provider for communicating with patients. Qualitative feedback indicated that participants intended to deepen their evaluation of menopause symptoms and more readily utilize evidence-based treatments within their practice and would like further information about action items for addressing inequity within their practice. Written feedback about the avatar experience was mixed.
Discussion: This multidisciplinary collaborative learning experience effectively increased the comfort and confidence of participants in addressing common menopause-related concerns which span the traditional silos of medical care, and increased awareness of racial and ethnic disparities. Interdisciplinary education may be an effective tool to promote patient-centered care and interdisciplinary collaboration.

