Psychopharmacology and Toxicology
Session: Poster Session
(139) A Curious Case of Self Amputation and Psychosis with Response to Clozapine
Trainee Involvement: Yes

Abram Davidov, MD
Psychiatry Resident
Wayne State University
Detroit, Michigan, United States
Firas Jadaan, MD
Psychiatry Resident
The Ohio State University
Columbus, Ohio, United States
Shazadie Soka, MD
Consultation Liaison Psychiatry Fellow
The Ohio State University Wexner Medical Center
Columbus, Ohio, United States- ES
Eleonora s. Sikic-Klisovic, MD, DFAPA
Associate Professor Clinical Psychiatry
The Ohio State University
Columbus, Ohio, United States
Presenting Author(s)
Co-Author(s)
Co-Author(s)
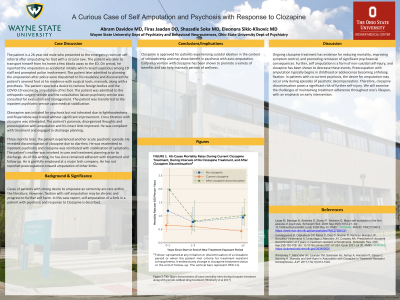
Background/Significance: Cases of patients with strong desire to amputate an extremity are rare. However, fixation with self amputation may be chronic and progress to further self harm. In this case report, self amputation of a limb in a patient with psychosis and response to Clozapine is described. Olanzapine was initiated for psychosis but not tolerated due to lightheadedness and Risperidone was trialed without significant improvement. Cross titration with Clozapine was attempted. The patient’s paranoia, disorganized thoughts and preoccupation with amputation and his intact limb improved. He was compliant with treatment and engaged in discharge planning. Three months later, the patient experienced another acute psychotic episode. He revealed discontinuation of clozapine due to diarrhea. He was readmitted to inpatient psychiatry and clozapine was reinitiated with stabilization of symptoms. The patient’s mother was involved in care and treatment planning prior to discharge. As of this writing, he has since remained adherent with treatment and follow up. He is gainfully employed at a major tech company. He has not reported preoccupations toward amputation of other limbs. Ongoing clozapine treatment has evidence for reducing mortality, improving symptom control, and promoting remission of significant psychosocial consequences. Further, self amputation is a form of non-suicidal self-injury, and clozapine has been shown to decrease these events. Preoccupation with amputation typically begins in childhood or adolescence becoming a lifelong fixation. In patients with co-current psychosis, the desire for amputation may occur only during episodes of psychotic decompensation. Therefore, clozapine discontinuation poses a significant risk of further self-injury. We will examine the challenges of maintaining treatment adherence throughout one's lifespan, with an emphasis on early intervention. Conclusions/Implications: Clozapine is approved for patients experiencing suicidal ideation in the context of schizophrenia and may show benefit in psychosis with auto amputation. Early intervention with clozapine has been shown to promote a variety of benefits, and can help maintain periods of wellness. Large M, Babidge N, Andrews D, Storey P, Nielssen O. Major self-mutilation in the first episode of psychosis. Schizophr Bull. 2009 Sep;35(5):1012-21. doi: 10.1093/schbul/sbn040. Epub 2008 May 20. PMID: 18495646; PMCID: PMC2728813. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2728813/) Iruretagoyena B, Castañeda CP, Mena C, Diaz C, Nachar R, Ramirez-Mahaluf JP, González-Valderrama A, Undurraga J, Maccabe JH, Crossley NA. Predictors of clozapine discontinuation at 2 years in treatment-resistant schizophrenia. Schizophr Res. 2021 Sep;235:102-108. doi: 10.1016/j.schres.2021.07.024. Epub 2021 Jul 30. PMID: 34340062.
Case:
The patient is a 26-year-old male who presented to the emergency room on self-referral after amputating his foot with a circular saw. The patient reported the amputation as accidental initially and later admitted to planning the amputation after police found the patient’s severed foot at his residence with surgical tools, manuals, and a prosthesis. He reported a desire to remove foreign bodies and the COVID-19 vaccine by amputation of his foot. The patient was admitted to the orthopedic surgery service and CL psychiatry was consulted. The patient was transferred to the inpatient psychiatric service upon medical stabilization.
Discussion:
References:
(https://pubmed.ncbi.nlm.nih.gov/34340062/)

