Obesity, Nutrition, and Eating Disorders
Session: Poster Session
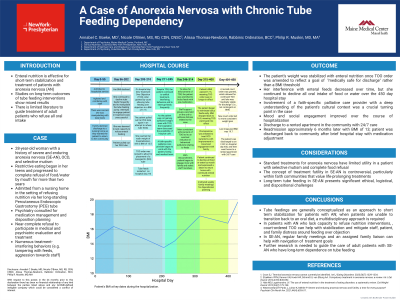
(112) A Case of Anorexia Nervosa with Chronic Tube Feeding Dependency
Trainee Involvement: Yes
- AB
Annabel C. Boeke, MD (she/her/hers)
Psychiatrist
Maine Medical Center
Portland, Maine, United States 
Nicole O'Brien, MS, RD, CDN, CNSC
Registered Dietitian
NewYork-Presbyterian / Columbia University Irving Medical Center
New York, New York, United States
Alissa Thomas-Newborn, Rabbinic Ordination, Board Certified Chaplain
Palliative Care Chaplain and Comprehensive Psychiatric Emergency Program Chaplain
New York-Presbyterian Columbia University Irving Medical Center
Teaneck, New Jersey, United States
Philip Muskin, MD, MA
Professor
Columbia University Irving Medical Center
New York, New York, United States
Presenting Author(s)
Co-Author(s)
Background: While tube feeding is often used as a short-term approach to nutritional rehabilitation in anorexia nervosa (AN), there is limited literature to guide treatment of patients who refuse all oral intake. We present a case of severe and enduring anorexia nervosa (SE-AN) in which the patient had declined all oral intake of food or water for years, demonstrated near-complete refusal to participate in evaluation and treatment, and was fully dependent on tube feedings, presenting significant logistical and dispositional challenges.
Case: A 28-year-old woman with a history of SE-AN, OCD, and selective mutism was admitted to the medical hospitalist service from a nursing home in the setting of refusing nutrition via her long-standing PEG tube. The patient had first developed restrictive eating in her teens; over several years, her symptoms progressed to complete refusal of any oral intake, in part due to an obsessional preoccupation with oral hygiene. She had spent most of her adulthood in institutional settings (eating disorder units and nursing homes); by the time of presentation to our hospital, she had been fully dependent on enteral nutrition for more than two years and had a BMI of 14.7. The case was complicated by selective mutism and near-complete refusal to interact with the medicine and psychiatry teams, which interfered with attempts to assess capacity and to engage the patient in behavioral treatment. The complex patient, family, and team dynamics of this case necessitated a multidisciplinary approach, with involvement of a faith-specific palliative care provider to liaise with family and extensive coordination between the medicine, psychiatry, nutrition, palliative care, ethics, nursing, social work, and legal teams. The patient was determined to lack capacity to refuse weight restoration and received court-ordered treatment over objection (TOO) with bolus tube feeds. The initial TOO was targeted to a BMI of 17.5; each time this goal was reached, the patient became obstructionist regarding feeding, leading her to repeatedly drop below the threshold BMI. A less specific goal was requested in a second hearing that resulted in weight stabilization. After over 14 months of medical hospitalization, she was discharged to a long-term care facility. Follow-up to be presented.
Discussion: There were several features of this case that were atypical for SE-AN, including near-complete refusal to communicate with the treatment team and refusal to take even water by mouth for multiple years. These atypical features precluded the use of standard interventions for AN, such as family-based treatment or cognitive behavioral therapy. Ultimately, successful stabilization required a multidisciplinary approach which included TOO, transition to bolus tube feeds, involvement of a faith-specific palliative care chaplain as a family liaison, and eventual adjustment of treatment goals to accept the need for long-term tube feedings.
Conclusion: Tube feedings are generally conceptualized as an approach to short term stabilization for patients with AN; when patients are unable to transition back to an oral diet, a multidisciplinary approach is required. Further research is needed to guide the care of adult patients with SE-AN who have long-term dependence on tube feeding.

