Transplant Psychiatry
Session: Poster Session
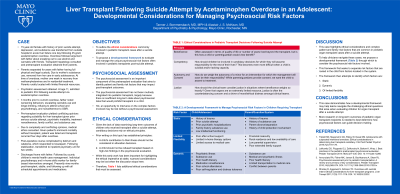
(203) A Developmental Framework to Manage Psychosocial Risk Factors in Children Requiring Organ Transplantation: A Case of an Adolescent Female Requiring Liver Transplant After a Suicide Attempt
Trainee Involvement: Yes
- TB
Tanner Bommersbach, MD (he/him/his)
Child and adolescent psychiatry fellow
Mayo Clinic
Rochester, Minnesota, United States - AM
Alastair McKean, MD
Assistant Professor of Psychiatry
Mayo Clinic
Rochester, Minnesota, United States
Presenting Author(s)
Co-Author(s)
Background/Significance:
The psychosocial assessment is an important component of the pretransplant evaluation that aims to identify risk factors that may impact post-transplant outcomes. However, there is a paucity of literature validating the psychosocial assessment in pediatric patients, especially in cases where the indication for transplantation is a suicide attempt (Triplett, 2019). This has led to a reliance on adult studies, despite the unique developmental and legal considerations that differentiate pediatric organ transplants from adults (Lefkowitz, 2014).
We discuss the case of a 15 year-old female who presented after an intentional acetaminophen overdose. Using this case, we first outline the ethical considerations commonly involved in pediatric transplant cases after a suicide attempt. We then propose a developmental framework to evaluate and manage the unique psychosocial risk factors involved. An adolescent female was transferred to our hospital in acute liver failure after an acetaminophen overdose. Transplant hepatology was consulted and information for the pretransplant psychosocial evaluation was obtained from the parents. The evaluation revealed risk factors involving both the child’s support system, including parental conflict, parental substance use, child protective services involvement, financial strain, and risk factors inherent to the patient, including prior suicide attempts, significant psychiatric comorbidity, recent substance use, and history of nonadherence with treatment. Given these risk factors, there was conflicting opinions amongst the treatment team regarding the patient’s suitability for transplantation, leading to ethics team consultation. Ultimately, the patient underwent liver transplantation. After medical stabilization, she was psychiatrically hospitalized and discharged from the hospital approximately one month after transplant. This case highlights ethical considerations that are common in pediatric organ transplant cases after a suicide attempt, including competency, consent (and assent), autonomy, beneficence, and justice. The case also includes common patient and family risk factors with which clinicians struggle when considering pediatric patients for transplantation. To help clinicians navigate these challenging cases, we propose a developmental framework to consider and manage the unique psychosocial risk factors involved. This framework first seeks to separate risk factors that are rooted in the child from factors that are located in the child’s system. The framework then attempts to identify which factors are 1) static, 2) dynamic, or of 3) limited flexibility (i.e. factors that may be modifiable through partnership with the patient and their support system). As is true for the case presented, we argue that much of the psychosocial risk for children after liver transplant falls into this latter category. Conclusions/Implications: This case exemplifies how a developmental framework may help teams navigate the challenging clinical and ethical questions that arise when evaluating a pediatric patient for organ transplant after a suicide attempt. More research on long-term outcomes of pediatric organ transplant recipients is needed to best determine how psychosocial factors can guide clinical decision-making. References Triplett KN, Mayersohn GS, Desai DM. Adolescents with suspected intentional overdose: Ethical considerations in determining liver transplant candidacy. Clinical practice in pediatric psychology. 2019; 7(2):170-178. Lefkowitz DS, Fitzgerald CJ, Wray J. Best practices in the pediatric pretransplant psychosocial evaluation. Pediatric Transplantation. 2014; 18:327–335.
Case:
Discussion:

