Psychopharmacology and Toxicology
Session: Poster Session
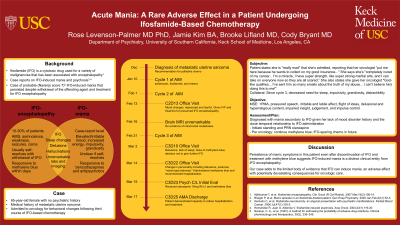
(141) Acute Mania: A Rare Adverse Effect in a Patient Undergoing Ifosfamide-Based Chemotherapy
Trainee Involvement: Yes

Rose Levenson-Palmer, MD PhD (she/her/hers)
Psychiatry Resident
Keck USC and LA General
Los Angeles, California, United States
Jamie Kim
Medical Student
Keck School of Medicine of USC
Los Angeles, California, United States
Brooke Lifland, MD (she/her/hers)
Clinical Assistant Professor of Psychiatry and the Behavioral Sciences
Keck School of Medicine of USC
SOUTH PASADENA, California, United States
Cody Bryant, MD
Assistant Program Director, USC/LAC+USC Consultation-Liaison Psychiatry Fellowship
University of Southern California
Los Angeles, California, United States
Presenting Author(s)
Co-Author(s)
Co-Author(s)
Background: Ifosfamide (IFO) is a cytotoxic, antineoplastic drug used to treat a variety of malignancies. It is associated with encephalopathy in 10-30% of patients, presenting with mental status changes, somnolence, weakness, hallucinations, coma, and seizures (Ajithkumar, 2007). There is limited literature on IFO-induced mania and psychosis, although both have been previously described in case reports (Brieger, 2000; Kerdudo, 2006; Hernandez, 2004). Here we present a case of probable (Naranjo score: 6) IFO-induced mania that persisted despite withdrawal of the offending agent and treatment for IFO encephalopathy.
Oncology continued methylene blue for IFO toxicity, with plans to initiate an IFO-sparing chemotherapy protocol once her mania resolved. Despite receiving multiple doses of methylene blue while hospitalized, her mania persisted. She was prescribed standing and PRN olanzapine, but only received a single dose due to refusals. Although she was quite ill, she was ultimately able to demonstrate capacity to decline psychotropic medications and psychiatric hospitalization. She was discharged under the care of her husband with strict return precautions in addition to a prescription for olanzapine and close medical follow-up. References Ajithkumar T, et al. Ifosfamide encephalopathy. Clin Oncol (R Coll Radiol). 2007 Mar;19(2):108-14. Brieger P, et al. Manic episode in an ifosfamide-treated patient. Gen Hosp Psychiatry. 2000 Jan-Feb;22(1):52-3. Kerdudo C, et al. Ifosfamide neurotoxicity: an atypical presentation with psychiatric manifestations. Pediatr Blood Cancer. 2006 Jul;47(1):100-2. Hernández R, Juan O, Alberola V. Ifosfamide-induced psychosis. Acta Oncol. 2004;43(1):119-20.
Case: A 65-year-old female with no psychiatric history and a medical history of metastatic uterine sarcoma was admitted to the oncology service for behavioral changes that started days after her second course of IFO-based chemotherapy one month prior. Further courses of IFO were canceled, and she received methylene blue to counteract presumed IFO encephalopathy. Unfortunately, her behavior progressively worsened. Her family reported that since the last IFO course, she had little need for sleep, highly impulsive behaviors, grandiosity, distractibility, aggression, and personality changes that represented a substantial change from baseline. Those symptoms were evident upon admission, with pressured speech and irritability making the interview difficult. She was diagnosed with mania secondary to IFO given her lack of mood disorder history and the close temporal relationship to IFO administration.
Discussion: This case of mania represents a rare and important potential adverse effect of IFO. Although IFO encephalopathy is more common, it typically self-resolves within three days of withdrawal of the medication, and can be treated with methylene blue, which has been shown to reverse IFO encephalopathy within minutes to days (Ajithkumar, 2007). Persistence of manic symptoms in this patient even after discontinuation of IFO and treatment with methylene blue suggests IFO-induced mania is a distinct clinical entity from IFO encephalopathy.
Conclusion: IFO is widely used in the treatment of many cancers and can have a variety of neuropsychiatric effects. Our case adds to the limited body of evidence that IFO can induce mania, an adverse effect with potentially devastating consequences for oncologic care.

