Psycho-Oncology and Palliative Care
Session: Poster Session
(131) Addressing Advanced Care Planning Difficulties in Patients with Terminal or Advanced Illness with Comorbid Mood Disorders and Suicidal Behavior
Trainee Involvement: Yes
- HK
Hannah Korman, MD
Psychiatry Resident
St. Elizabeths Hospital
Washington, District of Columbia, United States 
Paula Gomes Toledo Barros Costantino, MD
Psychiatrist Resident
Saint Elizabeths Hospital
ALEXANDRIA, Virginia, United States- AI
Ayyub Imtiaz, MD
Psychiatry Resident
Saint Elizabeths Hospital
Washington DC, District of Columbia, United States - ES
Enrico Suardi, MD, MSc., MA
Director of Psychiatry
Saint Elizabeths Hospital, DC Department of Behavioral Health
Washington, District of Columbia, United States
Presenting Author(s)
Co-Author(s)
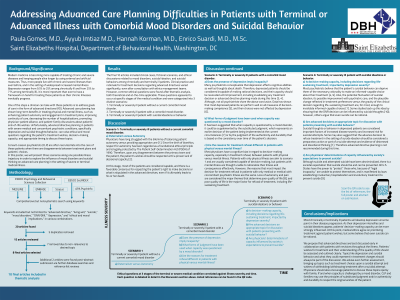
Background/Significance: Advanced directive (AD) planning in patients with severe medical and concomitant psychiatric conditions, specifically depression and suicidal thoughts/behavior, can raise ethical questions regarding the patient’s wishes for treatment, their decision-making capacity, and what is the appropriate timing to discuss these topics. Consult-Liaison psychiatrists (CLP) are often recruited late into the care of these patients when there are disagreements between treatment plans and patients’ choices. This poster aims to discuss these concerns using three scenarios in the illness trajectory. A comprehensive but nonsystematic search of multiple databases, including MEDLINE, EMBASE, Scopus, and APA PsychInfo was conducted. Specific keywords were used, such as “advanced directive,” “suicide,” “DNR/DNI,” and “depression,” in various combinations. Articles applicable to the topic underwent thematic analysis to determine underlying common concepts. The final 8 articles included cases and discussions related to mood disorders, suicidal ideation, and suicidal behaviors among chronically and terminally ill patients. Clinical rationale for treatment decisions regarding AD varied significantly, despite consultations with ethics management teams. No clear consensus on management was identified, but a trajectory of illness and common ethical questions, both theoretical and at-the-time applicable, arose at specific stages. Three discrete scenarios about AD planning and implementation were identified along the illness trajectory. These scenarios pertained to a terminally or severely ill patient: 1. Without a current comorbid mood disorder, 2. With a comorbid mood disorder, and 3. With suicidal ideations or behavior. The major ethical issue discussed within scenario 1 is paternalism versus autonomy, which is the professional dilemma of promoting patient autonomy versus providing appropriate care. There is a favorable consensus for respecting the patients’ decisions. Within scenario 2, the main question was: does depression invalidate capacity? Despite some data showing otherwise (Cotton, 1993), most articles share the opinion that depression can affect the rationality to make informed-capable choices. Lastly, scenario 3 discusses the impact of suicidal ideation on patients’ decisions regarding life-sustaining treatment (Lifton, 2000). Data suggests an impact, which may impose doubt about the appropriateness of AD planning at this time. Conclusions/Implications: Most chronically or terminally ill patients will usually develop depression at some point in their disease progression. As their depression intensifies and suicidal ideations appear, patients’ decision-making capacity can be more strongly influenced. At this point, medical ethics agree on prioritizing treatment against patient decisions, but some believe that even suicide can be rational. We propose that ADs are best discussed early in collaboration with patients with revisions throughout the illness. If and when capacity is challenged by a mood disorder, CLP and families may use the principles of authenticity and durability to respect the original wishes of the patient. Cotton P. Talk to people about dying--they can handle it, say geriatricians and patients. JAMA. 1993 Jan 20;269(3):321-2. Lifton I, Kettl PA. Suicidal ideation and the choice of advance directives by elderly persons with affective disorders. Psychiatr Serv. 2000 Nov;51(11):1447-9.
Methods:
Results:
Discussion:
References:

