Cardiology
Session: Poster Session
(003) Antipsychotics effects on PR, QRS, and QTc Intervals in Patients with Wolff-Parkinson-White Syndrome With and Without Cardiac Ablation
Trainee Involvement: Yes
.jpg)
Hassaan Gomaa, MD (he/him/his)
Consultation-Liaison attending psychiatrist
Albert Einstein Medical Center - Jefferson Health
Philadelphia, Pennsylvania, United States- SN
Sean Nutting, MD
Assistant professor of Psychiatry
Penn State College of Medicine
Hershey, Pennsylvania, United States - AC
Alonso Cortez-Resendiz, MD
Postdoctoral fellow
Penn State College of Medicine
Hershey, Pennsylvania, United States 
Charles Mormando, DO
Assistant Professor of Psychiatry
Penn State Hershey Medical Center
harrisburg, Pennsylvania, United States- AB
Alfredo Bellon, MD, PhD
Assistant professor of Psychiatry
Penn State College of Medicine
Hershey, Pennsylvania, United States
Presenting Author(s)
Co-Author(s)
1- Al-Khatib SM, Pritchett EL. Clinical features of Wolff-Parkinson-White syndrome. Am Heart J. 1999;138(3 Pt 1):403-413. 2- Qiu M, Lv B, Lin W, et. al. Sudden cardiac death due to the Wolff-Parkinson-White syndrome: A case report with genetic analysis. Medicine (Baltimore). 2018 Dec;97(51):e13248. 3- Nutting S, Martin C, Prensner R, et al. Antipsychotics for patients with Wolff-Parkinson-White Syndrome. Clin Schizophr Relat Psychoses. Jan 2019;doi:10.3371/CSRP.SNCM.121218
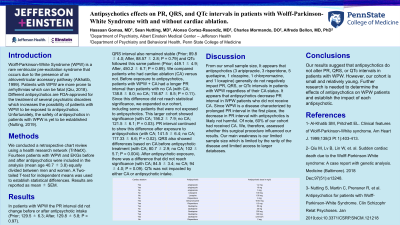
Background: Wolff-Parkinson-White Syndrome (WPW) is a rare ventricular pre-excitation syndrome that occurs due to the presence of an atrioventricular accessory pathway (Alkhatib, 1999). Patients with WPW are more prone to arrhythmias which can be fatal (Qiu, 2018). Different antipsychotics are FDA-approved for the treatment of several psychiatric disorders which increases the possibility of patients with WPW to be exposed to antipsychotics. Unfortunately, the safety of antipsychotics in patients with WPW is yet to be established (Nutting, 2019).
Methods: We conducted a retrospective chart review using a health research network (TriNetX). Fourteen patients with WPW and EKGs before and after antipsychotics were included in the analysis (mean age 40.7 ± 3.8) equally divided between men and women. A Two-tailed T-test for independent means was used to establish statistical differences. Results are reported as mean ± SEM.
Results: In patients with WPW the PR interval did not change before or after antipsychotic intake (Prior; 129.5 ± 6.3; After, 129.8 ± 5.8; P = 0.97). QRS interval also remained stable (Prior; 89.8 ± 4.0; After, 88.57 ± 2.8; P = 0.79) and QTc followed this same pattern (Prior; 449.1 ± 4.9; After, 450.2 ± 6.7; P = 0.89). However, 60% of our cohort had received cardiac ablation (CA). We, therefore, assessed whether this surgical procedure influenced our results. Before exposure to antipsychotics, patients with WPW + CA had a longer PR interval than patients with no CA (with CA; 138.8 ± 8.0; no CA; 118.67 ± 8.5; P = 0.11). Since this difference did not reach statistical significance, we expanded our cohort, including some patients that were not exposed to antipsychotics. This larger cohort did evidence significance (with CA; 156.2 ± 7.9; no CA; 121.5 ± 6.1; P = 0.03). PR interval continued to show this difference after exposure to antipsychotics (with CA; 141.5 ± 6.4; no CA; 117.33 ± 6.6; P = 0.02). QRS also showed differences based on CA before antipsychotic treatment (with CA; 80.7 ± 2.9; no CA; 102 ± 5.7; P = 0.004). After antipsychotic exposure, there was a difference that did not reach significance (with CA; 84.5 ± 3.4; no CA; 94 ± 4.0; P = 0.09). QTc was not impacted by either surgery or antipsychotic intake.
Conclusions: Our results suggest that antipsychotics do not alter PR, QRS, or QTc intervals in patients with WPW. However, our cohort is small and relatively young. Further research is needed to determine the effects of antipsychotics on WPW patients and establish the impact of each antipsychotic.
References:

