Catatonia
Session: Poster Session
(026) B12 Deficiency and Catatonia: A Case of Intrigue
Trainee Involvement: Yes
Stephen Marcoux, MD
Consultation-Liaison Psychiatry Fellow
University of Chicago Medical Center
Chicago, Illinois, United States- ZB
Zachary Bloomberg, MD
Resident Psychiatrist
University of Chicago
Chicago, Illinois, United States 
Margaret O'Brien, MD
Psychiatry Resident
University of Chicago, Department of Psychiatry and Behavioral Neuroscience
Chicago, Illinois, United States- mt
marie B. tobin, MD, FACLP
Professor of Psychiatry
University of Chicago
chicago, Illinois, United States
Presenting Author(s)
Co-Author(s)
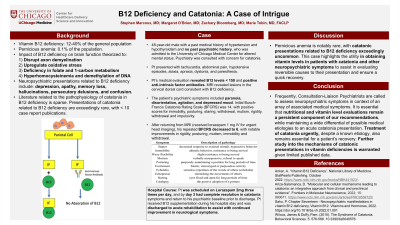
Pt presented with tachycardia, abdominal pain, hypotensive episodes, ataxia, apraxia, dystonia, and paresthesia. Pt’s medical evaluation was extensive and revealed B12 levels < 150, associated macrocytic anemia, and positive anti-intrinsic factor antibodies. MRI revealed lesions in the cervical dorsal cord consistent with B12 deficiency. The patient’s psychiatric symptoms included paranoia, disorientation, agitation, and depressed mood. The patient’s initial Busch-Francis Catatonia Rating Scale score was 6, with positive scores for immobility, posturing, staring, withdrawal, and impulsivity; this score occurred after a dose of Lorazepam was given for urgent head imaging. Pt was scheduled on Lorazepam 2mg three times per day, and by day 3 had complete resolution in catatonia symptoms and return to his psychiatric baseline prior to discharge. Pt received B12 supplementation during his hospital stay and was discharged to acute rehabilitation to assist with continued improvement in neurological symptoms. Conclusion- Frequently, Consultation-Liaison Psychiatrists are called to assess neuropsychiatric symptoms. It is essential that nutritional and vitamin level evaluations remain a persistent component of our recommendations, while maintaining a wide differential of possible medical etiologies to an acute catatonia presentation. Further study into the mechanisms of catatonic presentations in vitamin deficiencies is warranted given limited published data. Ankar, A. “Vitamin B12 Deficiency”. National Library of Medicine. StatPearls Publishing. October 2022. https://www.ncbi.nlm.nih.gov/books/NBK441923/. Ariza-Salamanca, D. “Molecular and cellular mechanisms leading to catatonia: an integrative approach from clinical and preclinical evidence”. Frontiers in Molecular Neuroscience, 2022; 15: 993671. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9558725/
Background: Vitamin B12 deficiency occurs in 12-40% of the general population, with pernicious anemia, a subtype involving anti-intrinsic factor antibodies, occurring in 0.1% of the population. The impact of B12 deficiency on brain function is theorized to disrupt axon demyelination and cause upregulation of oxidative stress. Neuropsychiatric presentations related to B12 deficiency include depression, memory loss, hallucinations, and confusion. Presentations of catatonia related to B12 deficiency are exceedingly rare, with < 10 case report publications. We report a case of a patient with altered mental status and subsequent catatonia, found to have B12 deficiency due to intrinsic factor blocking antibody after an exhaustive medical evaluation, with full resolution in catatonic symptoms after utilization of benzodiazepines. We aim to address the importance in completing a thorough medical evaluation in patients with catatonia to avoid misdiagnosis and delayed treatment.
Case: Pt is a 48-year-old male with a past medical history of hypertension and hypothyroidism and no past psychiatric history, who was admitted to a general medical unit for altered mental status. Psychiatry was consulted with concern for catatonia.
Discussion: Pernicious anemia is notably rare, with catatonic presentations related to B12 deficiency exceedingly uncommon. This case highlights the utility in obtaining vitamin levels in patients with catatonia and other neuropsychiatric symptoms to assist in evaluating reversible causes to their presentation and ensure quick recovery.
References:

