Psycho-Oncology and Palliative Care
Session: Poster Session
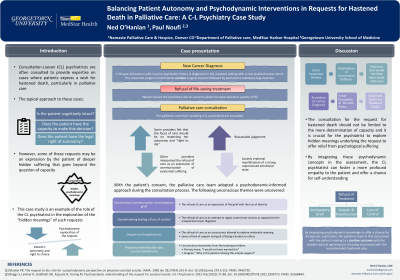
(130) Balancing Patient Autonomy and Psychodynamic Interventions in Requests for Hastened Death in Palliative Care: A C-L Psychiatry Case Study
Trainee Involvement: Yes

Edward O'Hanlan, LSW (he/him/his)
Hospice and Palliative Care Social Worker
Namaste Hospice and Palliative Care
Boulder , Colorado, United States.jpg)
Paul Noufi, MD
Medical Director, Palliative care section
MedStar Harbor Hospital, Georgetown University
Baltimore, Maryland, United States
Presenting Author(s)
Co-Author(s)
Consultation-Liaison (CL) psychiatrists are often consulted to provide expertise on cases where patients express a wish for hastened death, particularly in palliative care. While these requests are typically approached through a capacity evaluation, they may encompass broader issues that require further therapeutic exploration. This case study explores the complexities of these requests and examines the role of the CL psychiatrist in balancing patient autonomy with psychodynamic interventions to fully address the request's implications. A 58-year-old woman with no psychiatric history was diagnosed with localized rectal cancer and recommended to receive curative surgical excision followed by permanent colostomy bag insertion. Citing concerns about her post-operative quality of life, the patient refused the procedure and expressed a desire for hastened death. The palliative care team including a CL psychiatrist were consulted. On assessment, the patient had decision-making capacity; however, her request created a division among providers. Some argued that the focus should be on respecting the patient's autonomy. Others perceived the request as a communication of existential suffering and an opportunity to explore the patient’s grief and hopelessness. Team members were concerned that the patient’s distress was engendering in providers, by a process of projective identification, despair about the patient’s prognosis. With the patient's consent, the palliative team adopted a psychodynamic-informed approach to care. They uncovered anticipated grief and a strong "will-to-live" and continued to provide therapy over the following week to address the patient’s distress. As time progressed, the intensity of the patient's wishes for hastened death gradually decreased; she ultimately agreed to proceed with the recommended treatment plan. Upholding patients' bodily autonomy by avoiding imposing any burden of proof on them is a fundamental bioethical principle. However, when patients are in an acute existential crisis, the unconscious mobilization of psychological defenses may result in decisions that would not have been made otherwise. Requests for hastened death may then be verbalized. These consultations should not be limited to the determination of capacity and it is crucial for the psychiatrist to explore hidden meanings underlying the request to offer relief from psychological suffering. Paradoxically, these requests may be an unconscious attempt by the patient to seek a meaning to live. It is also vital to explore potential underlying concretized irrationality which could hinder the patient’s ability to appreciate their true prognosis. By integrating these psychodynamic concepts in the assessment, the CL psychiatrist can foster a more profound empathy to the patient and offer a chance for self-understanding. This psychodynamic approach also enables the establishment of a therapeutic relationship that allows for the exploration of countertransference reactions and enactment exhibited by the consulting teams. This case study highlights the importance of the CL psychiatrist approaching requests for hastened death beyond a mere determination of capacity. By integrating psychodynamic knowledge to offer a chance for therapeutic exploration, the palliative team in this case joined with the patient, leading to a positive outcome with the patient not just agreeing but choosing to proceed with the recommended treatment plan.
Background:
Case:
Discussion:
Conclusion:

