Psycho-Oncology and Palliative Care
Session: Poster Session
(132) Considerations for Transitioning to Palliative-oriented Care in Serious Mental Illness: A Case Study
Trainee Involvement: Yes

Robert E. Simons, MD
Psychiatry Resident
Temple University Hospital
Philadelphia, Pennsylvania, United States
Ryan Serdenes, DO
Fellow
Johns Hopkins Hospital
Baltimore, Maryland, United States- EL
Eric J. Lee, MD
Psychiatry Resident
Temple University Hospital
Philadelphia, Pennsylvania, United States - JK
Jessica Kovach, MD
Chair, Department of Psychiatry and Behavioral Sciences
Lewis Katz School of Medicine at Temple University
Philadelphia, Pennsylvania, United States 
Seetha Chandrasekhara, MD
Assistant Professor of Clinical Psychiatry
Lewis Katz School of Medicine at Temple University
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Co-Author(s)
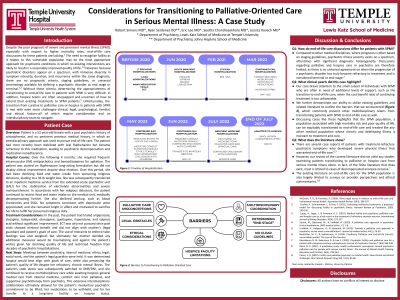
Background/Significance: Goals of care discussions for individuals with severe and persistent mental illness (SPMI) are medically and ethically complex. The possibility that treatment is interfering with a patient's quality of life can be especially challenging to consider in psychiatry, and in turn, the role of palliative medicine is often overlooked (Strand, 2020). Currently there are no guidelines outlining when patients with SPMI should be transitioned to a palliative approach (Coulter, 2021). Therefore, there remains considerable difficulty navigating end-of-life care in SPMI. Conclusion/Implications: Our consultation-liaison service helped transition this patient with schizophrenia to hospice care. This decision required extensive collaboration with the patient, legal guardian, hospital ethics committee, palliative medicine, hospitalists, and social work—a true interdisciplinary approach. It is our hope that this case highlights common barriers experienced when transitioning to palliative-oriented care in SPMI so that teams caring for these individuals are better equipped to navigate their end-of-life care more equitably.
Case: We present the case of a 52-year-old female with schizophrenia where an interdisciplinary approach was used to pursue end-of-life care. The patient was transferred to inpatient medicine from an extended acute psychiatric unit for electrolyte abnormalities and cachexia after restricting oral intake in the context of profound religious delusions instructing her to end her life. She had spent much of her adult life in psychiatric hospitals with limited improvement despite prolonged antipsychotic trials (including clozapine and multiple augmentation strategies) and ECT. The use of restraints to enforce tube feedings was discussed given her persistent malnourishment; however, the patient’s mother (legal guardian) decided such measures would be traumatizing and unlikely to yield substantial improvement. After extensive interdisciplinary collaboration, the patient was transferred to inpatient hospice.
Discussion: Compared to other medical disciplines, where prognosis is often based on staging guidelines, psychiatric illness severity exists on a spectrum, oftentimes with significant diagnostic heterogeneity. Discussions regarding palliative care in psychiatry are therefore limited, as there is no universal agreement on when the progression of a psychiatric disorder has truly become refractory to treatment and is considered terminal or end-stage (Coulter, 2021). Severe cases of anorexia nervosa (AN) comprise most of the psychiatric literature involving treatment cessation and a shift to palliative care, as AN can lead to significant medical comorbidities and possibly death (Rosenbaum, 2022). Even more, palliative care and hospice teams may feel unequipped to manage these patients. Navigating end-of-life care for individuals with SPMI is therefore extremely challenging and requires consideration of clinical, legal, and ethical factors to successfully integrate palliative care.
References:
Strand, M., Sjöstrand, M., & Lindblad, A. (2020). A palliative care approach in psychiatry: clinical implications. BMC Medical Ethics, 21(1), 1-8.
Coulter, A., Schuermeyer, I., & Sola, C. (2021). Evaluating Ineffective Treatments: A Proposed Model for Discussing Futility in Psychiatric Illness. Harvard Review of Psychiatry, 29(3), 240-245.
Rosenbaum D. M. Robertson D. & Law S. (2022). Psychiatric futility and palliative care for a patient with clozapine-resistant schizophrenia. Journal of Psychiatric Practice® 28(4) 344-348.

