Neurocognitive Disorders, Delirium, and Neuropsychiatry
Session: Poster Session
(087) Delirium, Dementia, or Schizophrenia: A Case Report and Literature Review of New-onset Psychosis in a Geriatric Patient
Trainee Involvement: Yes

Grace L. Johnson, BA (she/her/hers)
Medical Student
Mayo Clinic
Rochester, Minnesota, United States- KP
Kemuel Philbrick, MD
Hospital C/L Psychiatry Service
Mayo Clinic
Rochester, Minnesota, United States - CS
Christopher Sola, DO, FACLP
Consultation-Liaison Psychiatrist
Mayo Clinic
Rochester, Minnesota, United States
Presenting Author(s)
Co-Author(s)
Castle DJ, Murray RM. The epidemiology of late-onset schizophrenia. Schizophr Bull. 1993;19(4):691-700. doi: 10.1093/schbul/19.4.691. PMID: 8303220. Chen L, Selvendra A, Stewart A, Castle D. Risk factors in early and late onset schizophrenia. Compr Psychiatry. 2018 Jan;80:155-162. doi: 10.1016/j.comppsych.2017.09.009. Epub 2017 Sep 20. PMID: 29096206. Howard R, Rabins PV, Seeman MV, Jeste DV. Late-onset schizophrenia and very-late-onset schizophrenia-like psychosis: an international consensus. The International Late-Onset Schizophrenia Group. Am J Psychiatry. 2000 Feb;157(2):172-8. doi: 10.1176/appi.ajp.157.2.172. PMID: 10671383.
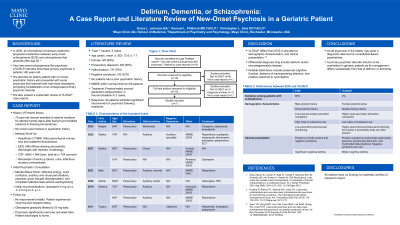
Background: It is estimated that 3% of patients with first-break primary psychosis present after age 60 (Castle, 1993), a phenomenon termed very late-onset schizophrenia-like psychosis (VLOSLP). VLOSLP is distinct from early-onset schizophrenia (EOS) in its background risk factors and clinical presentation (Howard, 2000). We describe an elderly patient with no known psychiatric history who presented with acute psychosis that resolved with high-dose olanzapine, prompting consideration of an undiagnosed primary psychotic disorder. We then present a systematic review of VLOSLP case reports.
Case: A 75-year-old woman was brought to the Emergency Department by ambulance for altered mental status after being found huddled outdoors in freezing temperatures, prompting admission to internal medicine. Review of available records revealed no previous similar symptoms, and the patient’s gross thought disorganization precluded reliable history collection. Mental status examination was notable for insomnia, affective energy, overt confusion, auditory and visual perturbations, paranoia, and gross thought disorganization. Head imaging (CT and MRI) revealed only mild parenchymal volume loss and scattered leukoaraiosis. Abeta42 was 886 and total tau was 104. Continuous EEG demonstrated diffuse slowing and periodic discharges with triphasic morphology. Olanzapine 5 mg at bedtime was started for symptomatic control and gradually titrated to 20 mg daily. Eventually, we obtained collateral from a family member, who described no previous contact with psychiatry and stable employment until retiring at age 55. In the decade prior to this presentation, however, she had become increasingly isolated. Two weeks after initiation of olanzapine and one week after the increased dose, her psychosis significantly improved, and she was discharged home.
Discussion: The etiology of our patient’s psychosis was uncertain. Head imaging and a low Abeta42 suggested neurodegeneration; however, her total tau was normal. EEG findings suggested delirium, but our patient was consistently alert. An underlying psychiatric disorder was suspected given her symptomatology and possible prodrome. A PubMed search of VLOSLP identified 6 case reports detailing a total of 8 cases (7/8 in females). Presentations were characterized by positive symptoms, including persecutory delusions (7/8) and auditory hallucinations (5/8). Previous literature indicates that patients with VLOSLP demonstrate better psychosocial functioning prior to disease onset compared to patients with EOS (Chen, 2018). VLOSLP lacks formal diagnostic criteria, but its background risk factors and clinical characteristics are consistent with our patient’s presentation. Ultimately, longitudinal follow-up with an outpatient psychiatric provider is necessary to determine a final diagnosis.
Conclusion: Acute psychosis in the elderly may pose a diagnostic dilemma. A primary psychotic disorder should not be overlooked in geriatric patients as its management differs substantially from that of delirium or dementia.
References:

