Systems-Based Practice and Administrative Psychiatry
Session: Poster Session
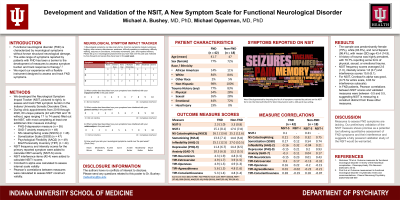
(184) Development and Validation of the NSIT, A New Symptom Scale for Functional Neurological Disorder
Trainee Involvement: No
.jpg)
Michael A. Bushey, MD, PhD
Assistant Professor of Psychiatry
Indiana University School of Medicine
Indianapolis, Indiana, United States- MO
Michael Opperman, M.D., Ph.D.
Assistan Professor
Central Michigan University
Saginaw, Michigan, United States
Presenting Author(s)
Co-Author(s)
Background/Significance: Functional neurological disorder (FND) is characterized by neurological symptoms (i.e. deficits in motor, sensory, and/or cognitive function) not caused by underlying structural neurological damage. The range of symptoms reported by patients with FND has been a barrier to the development of measures to assess symptom severity and track response to therapy (1,2). We report our experience with a flexible instrument developed to assess and track FND symptoms. 1. Nicholson TR et al. Outcome measures for functional neurological disorder: A review of the theoretical complexities. J Neuropsychiatry Clin Neurosci. 2020;32(1):33-42. doi:10.1176/appi.neuropsych.19060128 2. Pick S et al. Outcome measurement in functional neurological disorder: A systematic review and recommendations. J Neurol Neurosurg Psychiatry. 2020;91(6):638-649. doi:10.1136/jnnp-2019-322180
Methods: The Indiana University Somatic Disorders Clinic specializes in the treatment of Somatic Disorders, especially FND. To assess severity of FND symptoms, we developed the Neurological Symptom Impact Tracker (NSIT), which asks respondents to list up to three neurological symptoms that have occurred over the past year into a free text field. For each symptom reported, frequency is assessed with a 0-3 Likert scale (“none, several days, every day, multiple times/day”), and intensity is assessed with a 0-2 Likert scale (“mild”, “moderate”, “severe”). Three symptom interference items, scored on a 0–10-point Likert scale, assess interference with enjoyment of life, general activity, and relationships. During clinic appointments from 2018 through 2020, 61 patients (whose ages ranged from 17 years to 74 years) filled out the NSIT, with most completing at least one additional clinic measure (e.g., PHQ-9 depression measure (n = 55), GAD-7 anxiety measure (n = 49), Symptom Catastrophizing scale (n = 46), Somatic Symptom Scale (SSS8) (n = 47), psychological flexibility measure (AAQ2) (n = 49), and Ten-Item Personality Inventory (n = 44). We report summative data on patient demographics and scale outcomes. To assess preliminary validation of our NSIT measure, we calculated Cronbach’s alpha to assess internal scale validity, and Pearson’s correlations between measures to assess construct validity. This retrospective chart review was deemed exempt research by the Indiana University IRB.
Results: The sample was predominantly female (75%), white (83.6%), and non-Hispanic (98.4%), with mean (SD) age 43.4 (14.9). A history of trauma was highly prevalent, with 78.7% reporting some form of physical, sexual, or emotional trauma. NSIT frequency scores averaged 2.6 (1.0), intensity scores 1.8 (0.7) and interference scores 15.8 (8.1). For NSIT, Cronbach’s alpha was good, (0.73 for entire scale, 0.83 for interference subscale). In FND patients, Pearson correlations between NSIT scores and validated measures were between -0.5 and 0.5, suggesting NSIT is measuring a construct distinct from these other measures.
Discussion: Measures to assess FND symptoms are lacking. Our preliminary validation of the NSIT measure shows promise as a potential tool allowing quantitative assessment of FND symptoms and their interference and suggests a fully powered validation study of the NSIT would be warranted.
Conclusion: The NSIT is a new and flexible FND questionnaire with promising psychometric properties from a sample of clinic patients representing a broad age range.
References:

