Catatonia
Session: Poster Session
(013) Don't Hold Your Breath: A Case of Catatonia With Compulsive Breath-Holding Leading to Pneumomediastinum
Trainee Involvement: Yes

Connie Scoggins, BS (she/her/hers)
Medical student
Duke University
Durham, North Carolina, United States
Morgan M. Nakatani, BA (she/her/hers)
Medical Student
Duke University
Durham, North Carolina, United States- AT
Andrew Tuck, MD
Psychiatry Resident (PGY-4)
Duke University Health System
Durham, North Carolina, United States - JP
Julie Penzner, MD
Vice Chair, Education
Duke University
Durham, North Carolina, United States - JF
Jacob Feigal, MD
Assistant Professor
Duke University School of Medicine
Durham, North Carolina, United States 
Gregg A. Robbins-Welty, MD, MS
Chief Resident, Internal Medicine & Psychiatry
Duke University Hospital
Durham, North Carolina, United States
Presenting Author(s)
Co-Author(s)
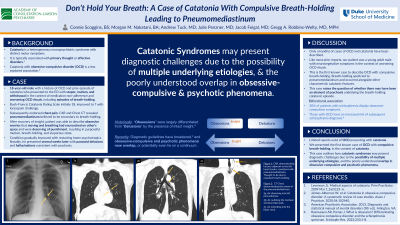
Background/Significance: Catatonia is a heterogeneous neuropsychiatric syndrome characterized by distinct motor symptoms. It is typically associated with primary thought or severe affective disorders in addition to various non-psychiatric conditions (Levenson, 2009). Catatonia with obsessive-compulsive disorder (OCD) is a less explored association in the literature (Jaimes-Albornoz, 2020). Here we present a case of OCD and catatonic stupor with compulsive breath-holding, resulting in pneumomediastinum. Case: Mr. X is an 18-year-old male with a psychiatric history of OCD and a prior episode of catatonia who presented with stupor, mutism, and withdrawal in the context of medication non-adherence and worsening OCD rituals, including episodes of breath-holding. On presentation, his Bush-Francis Catatonia Rating Scale (BFCRS) was 18. The patient’s catatonia improved with lorazepam administration. He subsequently endorsed chest pain, and imaging revealed pneumomediastinum believed to be secondary to breath-holding. With ongoing treatment and recovery of insight, the patient was able to describe obsessive worries that his moving and breathing had encroached on other’s space and were deserving of punishment. Eventually, this was followed by purposeful mutism, breath-holding, and stuporous state. His condition gradually improved with restarting home psychotropics. Notably, he presented several weeks later with paranoid delusions and hallucinations consistent with psychosis. Discussion: Only a handful of cases of OCD and catatonia have been described. Similar to other reports, our patient was a young adult male who presented with neurovegetative symptoms in the context of worsening OCD rituals. This is the first known case, however, to describe OCD with compulsive breath-holding. Symptoms were so severe that they led to pneumomediastinum, and made further unique in that they occurred alongside catatonia. This case raises the question of whether there may have been an element of psychosis underlying the breath-holding catatonic episode. “Obsessions” have historically been differentiated from “delusions” based largely on the presence of intact insight (Rasmussen and Parnas, 2022). However recent diagnostic guidelines have broadened (APA, 2013), and obsessive-compulsive and psychotic phenomena now overlap, or potentially even lie on a continuum. This is reflected in the fact that 30% of patients with schizophrenia display obsessive-compulsive symptoms, and those with OCD have an increased risk of subsequent schizophrenia diagnosis (Rasmussen and Parnas, 2022). Our case highlights the potential challenges associated with discerning the primary psychiatric cause of catatonia, especially when the underlying etiology may be multifactorial. Conclusion/Implications: There have been limited reports of OCD presenting with catatonia. Here we presented the first known case of OCD with features of compulsive breath-holding, in the context of catatonia. This case outlines how catatonic syndromes may present diagnostic challenges due to the possibility of multiple underlying etiologies, and the poorly understood overlap in obsessive-compulsive and psychotic phenomena. References: Levenson JL. Medical aspects of catatonia. Prim Psychiatry. 2009 Mar 1;16(3):23–6. Jaimes-Albornoz W, et al. Catatonia in obsessive-compulsive disorder: A systematic review of case studies. Asian J Psychiatr. 2020;54:102440. American Psychiatric Association. 2013. Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA.

