Obesity, Nutrition, and Eating Disorders
Session: Poster Session
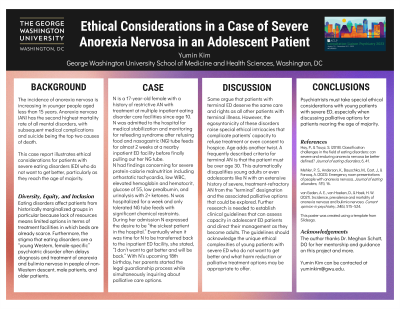
(117) Ethical Considerations in a Case of Severe Anorexia Nervosa in an Adolescent Patient
Trainee Involvement: Yes
Yumin Kim (she/her/hers)
Medical Student
George Washington University School of Medicine and Health Sciences
Vienna, Virginia, United States
Presenting Author(s)
Background/Significance: The incidence of anorexia nervosa is increasing in younger people aged < 15 years. Anorexia nervosa (AN) has the second highest mortality rate of all mental disorders, with subsequent medical complications and suicide being the top two causes of death. This case report illustrates ethical considerations for patients with severe eating disorders (ED) who do not want to get better, particularly as they reach the age of majority. Case: N is a 17-year-old female with a history of restrictive AN with treatment at multiple inpatient eating disorder care facilities since age 10. N was admitted to the hospital for medical stabilization and monitoring for refeeding syndrome after refusing food and NG tube feeds for almost 2 weeks at a nearby inpatient ED facility before finally pulling out her NG tube. N had findings concerning for severe protein-calorie malnutrition including orthostatic tachycardia, low WBC, elevated H/H, glucose 55, low prealbumin, and UA with 2+ ketones. N was hospitalized for a week and only tolerated NG tube feeds with significant chemical restraints. During her admission N expressed the desire to be “the sickest patient in the hospital.” Eventually when it was time for N to be transferred back to the inpatient ED facility, she stated, “I don’t want to get better and will be back.” With N’s upcoming 18th birthday, her parents started the legal guardianship process while simultaneously inquiring about palliative care options. Discussion: Some argue that patients with terminal ED deserve the same care and rights as all other patients with terminal illness. However, the egosyntonicity of these disorders raise special ethical intricacies that complicate patients’ capacity to refuse treatment or even consent to hospice. Age adds another twist. A frequently described criteria for terminal AN is that the patient must be over age 30. This automatically disqualifies young adults or even adolescents like N with an extensive history of severe, treatment-refractory AN from the “terminal” designation and the associated palliative options that could be explored. Further research is needed to establish clinical guidelines that can assess capacity in adolescent ED patients and direct their management as they become adults. The guidelines should acknowledge the unique ethical complexities of young patients with severe ED who do not want to get better and what harm reduction or palliative treatment options may be appropriate to offer. Conclusions/Implications: Psychiatrists must take special ethical considerations with young patients with severe ED, especially when discussing palliative options for patients nearing the age of majority. References: Hay, P., & Touyz, S. (2018). Classification challenges in the field of eating disorders: can severe and enduring anorexia nervosa be better defined? Journal of eating disorders, 6, 41. https://doi.org/10.1186/s40337-018-0229-8 Mehler, P. S., Anderson, K., Bauschka, M., Cost, J., & Farooq, A. (2023). Emergency room presentations of people with anorexia nervosa. Journal of eating disorders, 11(1), 16. https://doi.org/10.1186/s40337-023-00742-x van Eeden, A. E., van Hoeken, D., & Hoek, H. W. (2021). Incidence, prevalence and mortality of anorexia nervosa and bulimia nervosa. Current opinion in psychiatry, 34(6), 515–524. https://doi.org/10.1097/YCO.0000000000000739

