COVID-19
Session: Poster Session
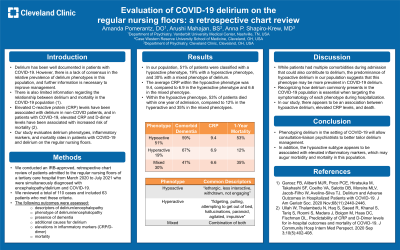
(059) Evaluation of COVID-19 Delirium on the Regular Nursing Floors: A Retrospective Chart Review
Trainee Involvement: Yes
Amanda Pomerantz, DO
Consultation-Liaison Psychiatry Fellow
Vanderbilt University Medical Center
Nashville, Tennessee, United States
Arushi Mahajan, BS (she/her/hers)
Medical student
Case Western Reserve University School of Medicine
Cleveland, Ohio, United States- AS
Anna P. Shapiro-Krew, MD
CL Psychiatry Associate Staff, Associate Program Director for CL Fellowship
Cleveland Clinic
Cleveland, Ohio, United States
Presenting Author(s)
Co-Author(s)
Background:
Delirium has been well documented in patients with COVID-19. However, there is a lack of consensus in the relative prevalence of delirium phenotypes in this population, and further information is necessary to improve management. There is also limited information regarding the relationship between delirium and mortality in the COVID-19 population (1). Elevated C-reactive protein (CRP) levels have been associated with delirium in non-COVID patients, and in patients with COVID-19, elevated CRP and D-dimer levels have been associated with increased risk of mortality (2). Our study evaluates delirium phenotypes, inflammatory markers, and mortality rates in patients with COVID-19 and delirium on the regular nursing floors.
Methods:
We conducted an IRB approved, retrospective chart review of patients admitted to the regular nursing floors of a tertiary care hospital from March 2020 to July 2021 who were simultaneously diagnosed with encephalopathy/delirium and COVID-19. We reviewed a total of 110 cases and included 63 patients who met these criteria. The following outcomes were assessed: descriptions of delirium/encephalopathy, phenotype of delirium/encephalopathy, presence of dementia, additional causes for delirium, elevations in inflammatory markers (CRP and D-dimer), and mortality.
Results:
In our population, 51% of patients were classified with a hypoactive phenotype, 19% with a hyperactive phenotype, and 30% with a mixed phenotype of delirium. The average CRP within the hypoactive phenotype was 9.4, compared to 6.9 in the hyperactive phenotype and 6.6 in the mixed phenotype. Within the hypoactive phenotype, 53% of patients died within one year of admission, compared to 12% in the hyperactive and 35% in the mixed phenotypes.
Discussion:
While patients had multiple comorbidities during admission that could also contribute to delirium, the predominance of hypoactive delirium in our population suggests that this phenotype may be more prevalent in COVID-19 delirium. Recognizing how delirium commonly presents in the COVID-19 population is essential when targeting the symptomatology of each phenotype during hospitalization. In our study, there appears to be an association between hypoactive delirium, elevated CRP levels, and death.
Conclusion:
Phenotyping delirium in the setting of COVID-19 will allow consultation-liaison psychiatrists to better tailor delirium management. In addition, the hypoactive subtype appears to be associated with elevated inflammatory markers, which may augur morbidity and mortality in this population.
References:
1) Garcez FB, Aliberti MJR, Poco PCE, Hiratsuka M, Takahashi SF, Coelho VA, Salotto DB, Moreira MLV, Jacob-Filho W, Avelino-Silva TJ. Delirium and Adverse Outcomes in Hospitalized Patients with COVID-19. J Am Geriatr Soc. 2020 Nov;68(11):2440-2446.
2) Ullah W, Thalambedu N, Haq S, Saeed R, Khanal S, Tariq S, Roomi S, Madara J, Boigon M, Haas DC, Fischman DL. Predictability of CRP and D-Dimer levels for in-hospital outcomes and mortality of COVID-19. J Community Hosp Intern Med Perspect. 2020 Sep 3;10(5):402-408. doi: 10.1080/20009666.2020.1798141. PMID: 33235672; PMCID: PMC7671719.

