COVID-19
Session: Poster Session
(062) Examining Barriers and Facilitators of COVID-19 Vaccination in an Acute Care Psychiatric Setting
Trainee Involvement: No

Allison Hadley, MD (she/her/hers)
Associate Professor
Oregon Health & Science University
Portland, Oregon, United States
Kristine Simpson, DNP (she/her/hers)
Assistant Professor
Oregon Health & Science University
Portland, Oregon, United States
Megan Cahn, PhD
Associate Scientist, Population Health
Legacy Health
Portland, Oregon, United States- AG
Anne Gross, MD, FACLP
Associate Professor
Oregon Health & Science University
Portland, Oregon, United States - JK
James Koved, MD
Assistant Professor and Co-Medical Director
Oregon Health & Science University
Portland, Oregon, United States
Presenting Author(s)
Co-Author(s)
Co-Author(s)
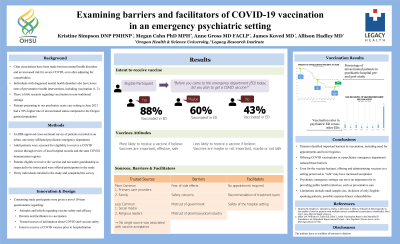
Background Clear associations have been made between mental health disorders and an increased risk for severe COVID, even after adjusting for comorbidities. Studies have also demonstrated lower rates of preventative health interventions, including vaccination, in patients with diagnosed mental disorders (Domino, Miles). Patients presenting to our psychiatric acute care setting in June 2021 had a 39% higher rate of unvaccinated status compared to the general Oregon population. Methods To better understand the attitudes, barriers and facilitators regarding COVID vaccination among individuals presenting to the Psychiatric Emergency Services (PES), we conducted an IRB-approved cross-sectional survey of patients recruited in the emergency room in a large, urban psychiatric hospital. Inclusion criteria included adult patients who were eligible to receive a COVID vaccine. Consenting study participants were given a novel 10-item questionnaire examining attitudes, beliefs, barriers, and facilitators to vaccination. Participants were asked about their previous intention to receive a COVID vaccine and were offered vaccination. Results Thirty individuals enrolled in the study and completed the survey. Of participants who had planned to receive a COVID vaccine but had not yet done so, 88% went on to be vaccinated in the PES. 60% of those who were undecided and 43% of those who had previously decided against receiving went on to be vaccinated. All participants thought vaccines were at least maybe effective. Participants were more likely to receive a vaccine in the PES if they agreed that vaccines are safe and/or important in ending the pandemic. They were less likely to receive a vaccine if they believed vaccines were maybe or not safe, and/or maybe or not important. Primary Care Providers and family members were the most commonly cited sources of trusted information about COVID-19. There was no association between trusted sources and a patient’s likelihood of accepting vaccine. Concerns about side effects, vaccine safety, and mistrust of the government were the most cited barriers, while ease of access, treatment team recommendations, and safety of the hospital setting were the most cited facilitators of vaccination. Discussion By offering COVID vaccination in an acute care psychiatric setting we were able to increase vaccine uptake in this vulnerable population. Even among the vaccine hesitant, offering and administering vaccines in a setting perceived as “safe” may have increased acceptance. Study limitations include a small sample size, inclusion of only English-speaking patients, and possible response-biases vulnerabilities in the questionnaire. Conclusion/Implications Reducing logistical barriers through diversifying settings in which vaccination is offered may increase uptake. Future research should evaluate the feasibility and acceptance of other preventative health measures in the psychiatric acute care setting. References Domino M, Beadles C, Lichstein J, Farley J, Morrissey J, Ellis A, Dubard CA Heterogeneity in the quality of care for patients with multiple chronic conditions by psychiatric comorbidity. Med Care. 2014 Mar;52 Suppl 3:S101-9. Miles LW, Williams N, Luthy KE, Eden L. Adult Vaccination Rates in the Mentally Ill Population: An Outpatient Improvement Project. J Am Psychiatr Nurses Assoc. 2020 Mar/Apr;26(2):172-180.

