Women's Mental Health
Session: Poster Session
(207) Factitious Disorder in Pregnancy: When Should You Confront the Patient?
Trainee Involvement: Yes

Ashwin N. Karnik, MD
Fellow
University of Washington
Seattle, Washington, United States- SG
Sanika Gadkari, MD
Resident Physician
University of Washington
Seattle, Washington, United States 
Julia Ruark, MD, MPH
Clinical Assistant Professor
University of Washington
Seattle, Washington, United States
Presenting Author(s)
Co-Author(s)
Background Case Discussion Conclusions References Eastwood, S., & Bisson, J. I. (2008). Management of Factitious Disorders: A Systematic Review. Psychotherapy and Edi-Osagie, E., Hopkins, R. H., & Edi-Osagie, N. (1998). Munchausen’s Syndrome in Obstetricsand Gynecology. Obstetrical & Yates, G. C. R., & Feldman, M. D. (2016). Factitious disorder: a systematic review of 455 cases in the professional literature.
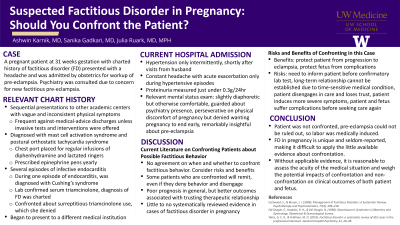
Factitious disorder (FD) in pregnancy is important to recognize because it can impact both patient and fetus. While there is research on when to confront a patient in FD (Eastwood, 2008), there is very little evidence on specifically pregnant patients (Yates 2016, Edi-Osagie 1998). We describe a case of FD in pregnancy, highlight its unique characteristics that make it difficult to apply literature evidence about confrontational approaches, and discuss the decision not to confront in this case.
Psychiatry was consulted by obstetrics for a patient at 31w1d gestation with a history of postural orthostatic tachycardia syndrome (POTS), mast cell activation syndrome (MCAS), anaphylaxis, and exogenous Cushing’s syndrome secondary to FD by surreptitious steroid use, admitted to antepartum for preeclampsia workup. Due to vacillating hypertension only when her partner visited, having a long-term port for infusion-based treatment of POTS and MCAS, access to prescriptions of epinephrine, records of laboratory confirmation of prior factitious disorder, and perseveration on no longer wanting to be pregnant, providers agreed on a diagnosis of factitious disorder. However, with reported acute headache and findings of hypertension and proteinuria, a simultaneous preeclampsia could not be excluded. The psychiatric interviewer elected not to ask her about FD behavior. Ultimately, she was diagnosed with preeclampsia with severe features, leading to preterm delivery and prolonged neonatal intensive care unit admission.
Available reviews, which largely exclude pregnant and by-proxy patients, show that either confrontational or non-confrontational approaches may be effective, but there is little evidence of factors that help determine which approach to choose in a particular case. However, when confrontation is used, there is a trend toward better outcomes with longer treatment courses (Eastwood, 2008). Several characteristics of the current case made this evidence difficult to apply—underreported condition (pregnancy), simultaneous self-imposed and by-proxy (fetus), and medical urgency and inability to provide a long treatment course. Therefore, a risk-benefit analysis was done. Since the risk of confrontation and the patient refusing treatment of preeclampsia outweighed the benefits of potentially continuing a normal pregnancy and minimizing preterm complications, non-confrontation and preterm delivery were done in the interest of both the patient and fetus.
FD in pregnancy is a unique and seldom-reported condition, making it difficult to apply the little available evidence about confrontation.
In the absence of applicable evidence, it is reasonable to assess the acuity of the medical situation and weigh the potential impacts of confrontation and non-confrontation on clinical outcomes of both patient and fetus.
Widespread recognition and reporting of FD in pregnancy should be encouraged in order to facilitate a future systematic review that could clarify recommendations around confrontation.
Psychosomatics, 77(4), 209–218.
Gynecological Survey.
General Hospital Psychiatry, 41, 20–28.

