Neurocognitive Disorders, Delirium, and Neuropsychiatry
Session: Poster Session
(105) Getting Under Your Skin: A Case of Diffuse Eczematous Dermatitis Presenting With Severe Hyperactive Delirium
Trainee Involvement: Yes

Sheela Vaswani, MD (she/her/hers)
Resident Physician
The Ohio State University Wexner Medical Center
Columbus, Ohio, United States- LT
Laura Taylor, DO
assistant professor
Ohio State University
Columbus, Ohio, United States .jpg)
David Kasick, MD, DFAPA, FACLP
Professor of Clinical Psychiatry and Behavioral Health
The Ohio State University Wexner Medical Center
Columbus, Ohio, United States
Presenting Author(s)
Co-Author(s)
This case illustrates the emerging awareness of the impact of circulating proinflammatory cytokines on the mind-skin interface through their potential to mediate severe, simultaneous behavioral and dermatologic pathology. Appreciating the psychiatric impact of systemic inflammation can reinforce bedside diagnostic precision as well as promote further understanding of the role of inflammation in the prevention and management of hyperactive delirium and other neuropsychiatric disorders.
Background: Increasing attention is being paid to the role of proinflammatory cytokines in mediating the onset of delirium and other neuropsychiatric conditions (Benros et al, 2014). Patients presenting with the combination of severe dermatoses and acute neurobehavioral changes demonstrate visible evidence of cytokine dysregulation across multiple organ systems. Accordingly, the impact of systemic inflammation and its treatments should be assessed carefully by the consulting psychiatrist in formulating the etiology and management of co-occurring behavioral disturbances.
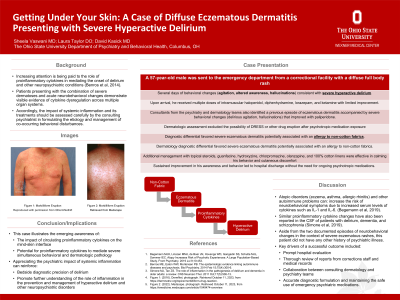
Case: A 57-year-old male was sent to the emergency department from a correctional facility with a diffuse full body rash and several days of behaviors (agitation, altered awareness, hallucinations) consistent with severe hyperactive delirium. Upon arrival, he received multiple doses of intramuscular haloperidol, diphenhydramine, lorazepam, and ketamine with limited improvement. Consultants from the psychiatry and dermatology teams also identified a previous episode of eczematous dermatitis accompanied by severe behavioral changes (delirious agitation, hallucinations) that improved with paliperidone. Dermatologic assessment excluded the possibility of DRESS or other drug eruption after psychotropic medication exposure, favoring severe eczematous dermatitis potentially associated with an allergy to non-cotton fabrics. Additional management with topical steroids, guanfacine, hydroxyzine, chlorpromazine, olanzapine, and 100% cotton linens were effective in calming his behavior and cutaneous discomfort. Sustained improvement in his awareness and behavior led to hospital discharge without the need for ongoing psychotropic medications.
Discussion: Atopic disorders (eczema, asthma, allergic rhinitis) and other autoimmune problems can increase the risk of neurobehavioral symptoms due to increased serum levels of cytokines such as IL-1 and IL-6. (Begemann, 2019). Similar proinflammatory cytokine changes have also been reported in the CSF of patients with delirium, dementia, and schizophrenia (Simone, 2019). Aside from two documented episodes of neurobehavioral changes in the context of severe eczematous rashes, this patient did not have any other history of psychiatric illness. Prompt hospital evaluation, thorough review of reports from corrections staff and medical records, as well as collaboration between consulting medical teams was critical in accurate diagnostic formulation and maintaining the safe use of emergency psychiatric medications.
Conclusion:
References:
Begemann MJH, Linszen MMJ, de Boer JN, Hovenga WD, Gangadin SS, Schutte MJL, Sommer IEC. Atopy Increases Risk of Psychotic Experiences: A Large Population-Based Study. Front Psychiatry. 2019 Jul 9;10:453.
Benros ME, Eaton WW, Mortensen PB. The epidemiologic evidence linking autoimmune diseases and psychosis. Biol Psychiatry. 2014 Feb 15;75(4):300-6.
Simone MJ, Tan ZS. The role of inflammation in the pathogenesis of delirium and dementia in older adults: a review. CNS Neurosci Ther. 2011 Oct;17(5):506-13.

