Transplant Psychiatry
Session: Poster Session
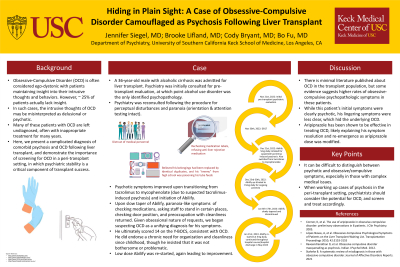
(198) Hiding in Plain Sight: A Case of Obsessive-Compulsive Disorder Camouflaged as Psychosis Following Liver Transplant
Trainee Involvement: Yes

Jennifer Siegel, MD (she/her/hers)
Psychiatry Resident
University of Southern California
Los Angeles, California, United States
Brooke Lifland, MD (she/her/hers)
Clinical Assistant Professor of Psychiatry and the Behavioral Sciences
Keck School of Medicine of USC
SOUTH PASADENA, California, United States
Cody Bryant, MD
Assistant Program Director, USC/LAC+USC Consultation-Liaison Psychiatry Fellowship
University of Southern California
Los Angeles, California, United States
Bo Fu, MD
Program Director, USC/LAC+USC Consultation Liaison Fellowship
USC Keck School of Medicine
Los Angeles, California, United States
Presenting Author(s)
Co-Author(s)
López-Navas, A, et al. Obsessive-Compulsive Psychological Symptoms of Patients on the Liver Transplant Waiting List. Transplantation Proceedings 2010; 42:3153-3155 Raveendranathan D, et al. Obsessive compulsive disorder masquerading as psychosis. Indian J Psychol Med. 2012. Stahnke B. A systematic review of misdiagnosis in those with obsessive-compulsive disorder. Journal of Affective Disorders Reports. 2021.
Background:
Obsessive-Compulsive Disorder (OCD) is often considered an ego-dystonic psychopathology in which patients find their symptoms distressing while maintaining insight into the excessive nature of their thoughts and behaviors. However, approximately 25% of patients actually lack insight. In such cases, the intrusive thoughts of OCD may be misinterpreted as delusional components of a psychotic disorder (Raveendranathan, 2012). Many patients with OCD are left undiagnosed, often with subsequent inappropriate treatment for many years (Stahnke, 2021).
Here, we present a complicated diagnosis of comorbid psychosis and OCD following liver transplant, and demonstrate the importance of screening for OCD in a peri-transplant setting, in which psychiatric stability is a critical component of transplant success.
Case:
A 36-year-old male with alcoholic cirrhosis was admitted for liver transplant. Psychiatry was initially consulted for pre-transplant evaluation, at which point alcohol use disorder was the only identified psychopathology. He subsequently received a liver transplant
Psychiatry was reconsulted following the procedure for perceptual disturbances and paranoia. He was frequently rechecking medication labels, endorsing significant distrust in medical personnel, and refusing anti-liver rejection medications. He also espoused delusional beliefs, including that his belongings had been replaced by identical duplicates, and his “enemy” from high school was poisoning his tube feeds. His orientation and attention testing remained impeccable throughout. Due to concern for tacrolimus-induced psychosis, he was transitioned to mycophenolate and started on aripiprazole. His psychotic symptoms quickly improved, and aripiprazole was slowly discontinued. Unfortunately, upon discontinuation, mild apparent paranoia returned, and low-dose aripiprazole was re-started, again leading to improvement.
His lingering symptoms included particularities with staff, checking medication packaging, asking staff to stand in certain places, and pre-occupation with cleanliness. While he did endorse a chronic need for organization and cleanliness since childhood, he insisted that it was not bothersome or problematic. He ultimately scored 14 on the Y-BOCS, consistent with OCD.
Discussion:
This case illustrates the potential for difficulty distinguishing between psychotic and obsessive/compulsive symptoms, especially in those with complex medical issues. There is minimal literature published about OCD in the transplant population, but some evidence suggests higher rates of obsessive-compulsive psychopathologic symptoms in these patients (López-Navas 2010). While this patient’s initial symptoms were clearly psychotic, his lingering symptoms were less clear, which obfuscated the underlying OCD. Aripiprazole has been shown to be effective in treating OCD (Connor, 2005), potentially explaining his symptom resolution and subsequent re-emergence. When working up cases of psychosis in the peri-transplant setting, psychiatrists should consider the potential for OCD, and screen and treat accordingly.
References:
Connor, K, et al. The use of aripiprazole in obsessive-compulsive disorder: preliminary observations in 8 patients. J Clin Psychiatry. 2005.

