Neurocognitive Disorders, Delirium, and Neuropsychiatry
Session: Poster Session
(101) Hyperactive Delirium in Heroin Toxic Leukoencephalopathy Complicated by Atypical NMS
Trainee Involvement: Yes
- PM
Pratheek Mangini, MD
Psychiatry Resident
Temple University Hospital
Philadelphia, Pennsylvania, United States 
Ryan Serdenes, DO
Fellow
Johns Hopkins Hospital
Baltimore, Maryland, United States.jpg)
Natalia Ortiz, MD DFAPA FACLP
Chief Consultation and Liaison Psychiatry
Lewis Katz Temple School of Medicine
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Co-Author(s)
Background: Heroin toxic leukoencephalopathy (HTLE) is rare cause of encephalopathy that can present with delirium, motor symptoms, and behavioral changes which may be misattributed to primary psychopathology (Al Chalabi, 2020). This case report discusses a patient whose diagnosis was unrecognized, resulting in polypharmacy, delayed treatment, and prolonged agitation.
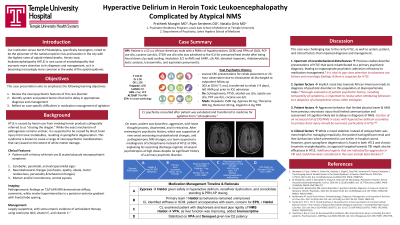
Case: The patient is a 52-year-old African American male with a past psychiatric history of alcohol use disorder, phencyclidine use disorder, and cocaine use disorder and past medical history of hypothyroidism and GERD who was admitted to the ICU after being found down and delirious from presumed heat stroke, whom psychiatry was consulted to manage agitation secondary to hyperactive delirium. The patient has a history of substance-induced psychosis, but atypically had a prolonged psychiatric hospitalization for one month prior to admission where they were placed on several high-dose psychotropic agents, discharged, and later found to have altered mental status resulting in current admission. MRI was obtained due to focal neurologic deficits found on exam and incidentally showed hallmark signs of HTLE. As the patient deescalated from the ICU to the floors, he became agitated and physically aggressive. Medication management was challenging as his hospital course was complicated by acute hypoxic respiratory failure, aspiration pneumonia, rhabdomyolysis, transaminitis, and lactic acidosis. Benzodiazepines resulted in worsened disinhibition, olanzapine was ineffective during acute agitation, and valproic acid was unable to be administered due to hepatic injury. Haloperidol was chosen as the primary agent to manage patient’s agitation as well as an antioxidant treatment for HTLE. Unfortunately, there was limited response to the antioxidant regimen and haloperidol, and thus, doses of antipsychotic were increased by primary team. The patient subsequently developed atypical neuroleptic malignant syndrome (NMS), exhibiting diaphoresis and lead pipe rigidity. Psychotropics were then discontinued, and bromocriptine was initiated. As transaminitis resolved, patient was cross tapered to valproic acid and had improvement of mental status.
Discussion: This case highlights the essential role of interdisciplinary collaboration in diagnosing and managing HTLE in setting of hyperactive delirium and multisystem organ failure. While Haloperidol has a significant body of literature detailing its safety and efficacy in hyperactive delirium, the patient's HTLE may have predisposed him to developing NMS (Maldonado, 2017; Serdenes, 2021). We will explore the system factors, clinical variables, and inter-team communication that can facilitate early diagnosis, management, and prevention of adverse outcomes in patients with HTLE.
References:
Al-Chalabi M, Lateef S, Gharaibeh K, Saraiya P, Ghannam M. Mimicking a Psychiatric Disorder: Heroin-Induced Leukoencephalopathy. Cureus. 2020 Oct 5;12(10):e10805. doi: 10.7759/cureus.10805. PMID: 33163309; PMCID: PMC7641477.
Maldonado JR. Acute Brain Failure: Pathophysiology, Diagnosis, Management, and Sequelae of Delirium. Crit Care Clin. 2017 Jul;33(3):461-519. doi: 10.1016/j.ccc.2017.03.013. PMID: 28601132.
Serdenes R, Orr S, Trio P, Chandrasekhara S, Musselman M. A Rare Case Report of a Corpus Callosal Splenial Lesion in the Context of Atypical Neuroleptic Malignant Syndrome. J Investig Med High Impact Case Rep. 2021 Jan-Dec;9:23247096211029751. doi: 10.1177/23247096211029751. PMID: 34229456; PMCID: PMC8267016.

