Psychopharmacology and Toxicology
Session: Poster Session
(150) Intravenous Ketamine Exacerbating Symptoms of Acute Stress Disorder: A Case Report and Systematic Review of Existing Literature
Trainee Involvement: Yes

Charalambia Louka, MD
Resident Psychiatrist
NewYork-Presbyterian/Weill Cornell Medical Center
New York, New York, United States- SC
Stephanie Chiao, MD
Assistant Professor of Clinical Psychiatry
NewYork-Presbyterian/Weill Cornell Medical Center
New York, New York, United States
Presenting Author(s)
Co-Author(s)
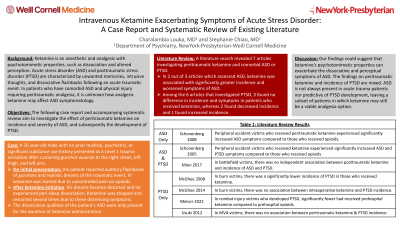
Background/Significance: Ketamine is an anesthetic and analgesic with psychotomimetic properties, such as dissociation and altered perception. Acute stress disorder (ASD) and posttraumatic stress disorder (PTSD) are characterized by unwanted memories, intrusive thoughts, and dissociative flashbacks following an acute traumatic event. In patients who have comorbid ASD and physical injury requiring peritraumatic analgesia, it is unknown how analgesic ketamine may affect ASD symptomatology. The following case report and accompanying systematic review investigate the effect of peritraumatic ketamine on incidence and severity of ASD, and subsequently the development of PTSD. Literature Review: A literature search revealed 7 articles investigating peritraumatic ketamine and comorbid ASD or PTSD. Studies measured incidence and severity of symptoms using a variety of clinical scales. In 2 out of 3 articles which assessed ASD, ketamine was associated with significantly greater incidence and worsened symptoms of ASD, particularly re-experiencing, dissociation, and avoidance. Among the 6 articles that investigated PTSD, 3 found no difference in incidence and symptoms in patients who received ketamine, whereas 2 found decreased incidence and 1 found increased incidence. These studies, however, also varied greatly in their methodologies and latency in measuring PTSD after the traumatic event. This literature review suggests that ketamine potentiates the psychological sequelae of trauma in the acute phase but not in the long term.
Case: A 26 year-old male with no prior medical, psychiatric, or significant substance use history presented as a Level 1 trauma activation after sustaining gunshot wounds to the right cheek, left thigh, and left arm. After waking up, the patient reported auditory flashbacks of gunshots and realistic dreams of the traumatic event. His pain was uncontrolled on opioids, so he was started on an intravenous (IV) ketamine drip. While on ketamine, his dreams became distorted and he experienced perisleep dissociation. Ketamine was stopped and restarted several times due to these distressing symptoms, despite the addition of as needed benzodiazepines. The dissociative qualities of the patient’s ASD were only present for the duration of ketamine administration.
Discussion: We do not fully understand how ketamine affects ASD, but given the findings in the above case and literature review, we theorize that ketamine’s psychotomimetic properties can exacerbate the dissociative and perceptual symptoms of ASD. The findings on peritraumatic ketamine and incidence of PTSD are mixed. ASD is not always present in acute trauma patients nor predictive of PTSD development, leaving a subset of patients in which ketamine may still be a viable analgesia option.
Implications: It is our suggestion that if ketamine is considered for a patient with acute trauma, providers should screen and monitor for ASD symptoms.

