Collaborative and Integrated Care
Session: Poster Session
(047) K-POP is Popular: A Novel Collaborative Care Approach in the Kidney Palliative Care Outpatient Psychiatry Clinic
Trainee Involvement: Yes

Celeste Peay, MD, JD (she/her/hers)
Consultation Liaison Fellow
Keck USC
Long Beach, California, United States
Fernando Espi-Forcen, MD, PhD
Instructor of Psychiatry at Harvard Medical School
Massachusetts General Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Co-Author(s)
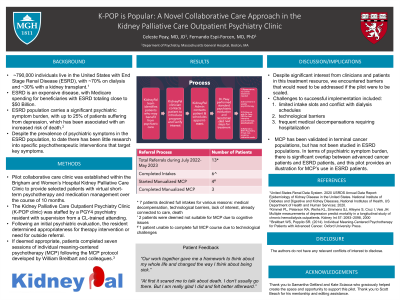
Background/Significance Approximately 790,000 individuals live in the United States with End Stage Renal Disease (ESRD), with ~70% on dialysis and ~30% with a kidney transplant.1 ESRD is an expensive disease, with Medicare spending for beneficiaries with ESRD totaling close to $50 Billion. This population also carries a significant psychiatric symptom burden, with up to 25% of patients suffering from depression, which has been associated with an increased risk of death.2 Despite the prevalence of psychiatric symptoms in the ESRD population, to date there has been little research into specific psychotherapeutic interventions that target key symptoms. A pilot collaborative care clinic was established within the Brigham and Women’s Hospital Kidney Palliative Care Clinic to provide selected patients with virtual short-term psychotherapy and medication management over the course of 10 months. The Kidney Palliative Care Outpatient Psychiatry Clinic (K-POP clinic) was staffed by a PGY4 psychiatry resident with supervision from a CL-trained attending. Following an initial psychiatric evaluation, the resident determined appropriateness for therapy intervention or need for outside referral. If deemed appropriate, patients completed seven sessions of individual meaning-centered psychotherapy (MCP) following the MCP protocol developed by William Breitbart and colleagues.3 During the pilot period, thirteen patients were referred for an initial evaluation, with seven completing the full intake. Of the seven intakes, five were deemed appropriate for MCP, with three patients completing a full course. There was significant attrition from referral to intake due to worsening medical illness, hospital admission, and one death. Two patients began MCP but did not complete it due to technological difficulty and medical decompensation. Within the Kidney Palliative care program, there was significant interest from clinicians and patients in this treatment resource despite the low number of successful referrals. There were several challenges to successful implementation including: 1) limited intake slots and conflict with dialysis schedules, 2) technological barriers, and 3) frequent medical decompensations requiring hospitalization. These barriers would need to be addressed if the pilot was to be scaled. MCP has been validated in terminal cancer populations, but has not been studied in ESRD populations. In terms of psychiatric symptom burden, there is significant overlap between advanced cancer patients and ESRD patients, and this pilot provides an illustration for MCP’s use in ESRD patients. The pilot clinic provided an additional resource for psychiatric referral, evaluation, and intervention. Furthermore, the clinic allowed a senior resident to gain experience and training in a brief therapy modality in a collaborative care setting. 1United States Renal Data System. 2020 USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States. National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, US Department of Health and Human Services; 2020. 2Kimmel PL, Peterson RA, Weihs KL, Simmens SJ, Alleyne S, Cruz I, Veis JH: Multiple measurements of depression predict mortality in a longitudinal study of chronic hemodialysis outpatients. Kidney Int 57: 2093–2098, 2000 3 Breitbart WS, Poppito SR. (2014). Individual Meaning-Centered Psychotherapy for Patients with Advanced Cancer. Oxford University Press.
Methods
Results
Discussion
Conclusion/Implications
References

