Quality and Safety
Session: Poster Session
(162) Management of Hospital Violence in High-Risk Patient Populations: Utilizing Brøset Violence Checklist with Proactive C-L Psychiatry Consultation
Trainee Involvement: Yes

Kathryne Adams, MD
Resident Physiatrist
Tufts Medical Center
Boston, Massachusetts, United States
Glenn Robison, BS
Medical Student
Tufts University School of Medicine
Boston, Massachusetts, United States
Isabelle Hashim, BA
Medical Student
Tufts University School of Medicine
Boston, Massachusetts, United States
Cristina Montalvo, MD, MBS
Chief, Consultation-Liaison and Emergency Psychiatry
Tufts Medical Center
Boston, Massachusetts, United States
Presenting Author(s)
Co-Author(s)
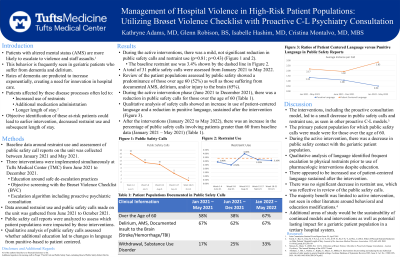
Patients with altered mental status create a complex situation for ongoing care, especially in regard to both staff and patient safety. This patient population is more likely to escalate to violence and staff assault (Joint Commission, 2018). While the spectrum of causes for altered mental status is broad, there is a substantial impact among the geriatric population who often suffer from dementia and delirium with rates of dementia anticipated to exponentially increase in an aging population. Patients affected by these disease processes often have increased use of restraints and additional medication administration, creating longer hospital lengths of stay (Kwox et al, 2012). The ability to objectively identify these at-risk patients and intervene could improve the quality of patient care as well as decrease the length of stay. At Tufts Medical Center (TMC), we worked to implement both new education and an objective screening tool, the Brøset Violence Checklist (BVC), with an escalation algorithm, leading to psychiatric consultation, to identify these patients prior to assaultive behavior. This project was approved by the TMC IRB. We anticipated that this proactive model would lead to decreased restraints and calls to security, as shown in similar proactive consultation models (Stinson et al, 2020). We found a decrease in both restraints usage and calls to security, down from 3.4% to 3.1% (ratio of restraint days over patient days) and 5 to 2 calls (weekly average). In a secondary review, we looked to assess specifically which patient population was benefiting the most. While this review is ongoing, it does appear that many affected were those over the age of 60. With ongoing analysis of security call reports, we anticipate that the language of the report may reflect attempts to limit physical restraints, reaffirming the impact of the education provided. Unfortunately, there was not a decrease in the length of stay, which remained around 5 days. This model and analysis of its effectiveness add to previous literature looking at interventions to reduce restraints in a geriatric population, which has found significant limitations to interventions such as increased education and behavioral modifications for patients and teams alone (Abraham et al, 2022). This shows that an objective assessment, education, and proactive consultation is an effective combination to provide safer care to the geriatric patient population. Abraham J, Hirt J, Richter C, Köpke S, Meyer G, Möhler R. Interventions for preventing and reducing the use of physical restraints of older people in general hospital settings. Cochrane Database of Systematic Reviews 2022, Issue 8. Art. No.: CD012476. DOI: 10.1002/14651858.CD012476.pub2. Joint Commission Sentinel Event Report Issue 59, April 2018 Kwok, T., Bai, X., Chui, M. Y. P., Lai, C. K. Y., Ho, D. W. H., Ho, F. K. Y., & Woo, J. (2012). Effect of Physical Restraint Reduction on Older Patients’ Hospital Length of Stay. Journal of the American Medical Directors Association, 13(7), 645–650. DOI: 10.1016/j.jamda.2012.05.019 Stinson, K., Dunn, T. (2020, Nov 12-13). Utilization of the Broset Violence Checklist to Proactively Engage Consultation-Liaison Psychiatry. The Annual Meeting of the ACLP. Virtual

