Collaborative and Integrated Care
Session: Poster Session
(049) Multidisciplinary Stabilization of Patient with Anorexia Nervosa in the Acute Setting
Trainee Involvement: Yes

Daniel Cabrera, MD-PhD
Psychiatry Resident
New York Presbyterian/Weill Cornell Medical Center
New York, New York, United States
Jihoon Ha, MD
Psychiatry Attending
New York Presbyterian/Weill Cornell Medical Center
New York, New York, United States
Presenting Author(s)
Co-Author(s)
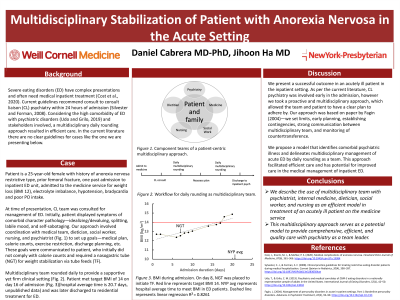
Background: Severe eating disorders (ED) have complex presentations and often need medical inpatient treatment (Cost et al., 2020). Current guidelines recommend consult to consult liaison (CL) psychiatry within 24 hours of admission (Silvester and Forman, 2008). Considering the high comorbidity of ED with psychiatric disorders (Udo and Grilo, 2019) and stakeholders involved, a multidisciplinary daily rounding approach resulted in efficient care. In the current literature there are no clear guidelines for cases like the one we are presenting below.
Case: Patient is a 25-year-old female with history of anorexia nervosa restrictive type, one past inpatient ED hospitalization, admitted to the medicine service due to low weight (BMI 12), hypotension, bradycardia, hypothermia, and electrolyte imbalance. Initially, patient displayed symptoms of comorbid character pathology—idealizing/devaluing, splitting, labile mood, and self-sabotaging. Our approach involved coordination with medical team, dietician, social worker, and nursing to set up goals—medical plan, calorie counts, exercise restriction, discharge planning, etc. These goals were communicated to patient at daily multidisciplinary rounds. Patient initially did not comply with calorie counts and required a nasogastric tube for weight stabilization. However initial resistance subsided, and patient met caloric needs without NG tube, eventually meeting target BMI of 14 on day 16 of admission, which is much shorter than average time for similar cases, 20.7 days (internal hospital data). Patient was later discharged to residential treatment for ED without medical complications.
Discussion: We present a successful outcome in an acutely ill ED patient in the inpatient medical setting. As per the current literature, CL was involved early, however we took a proactive and multidisciplinary approach, which allowed the team and patient to have a clear plan to adhere by. Our approach was based on paper by Fagin (2004)—we set limits, early planning, establishing contingencies, strong communication between multidisciplinary team, and monitoring of countertransference. We propose a model that identifies comorbid psychiatric illness and delineates multidisciplinary management of acute ED by daily rounding as a team. This approach facilitated efficient care and has potential for improved care in the medical management of inpatient ED.
Conclusion/Implications: We describe the use of daily multidisciplinary team rounds involving psychiatrist, internal medicine, dietician, social worker, and nursing as an efficient model in treatment of an acutely ill ED patient on the medicine service. This preliminary report serves a foundation for potential study of this intervention.
References:
Cost, J., Krantz, M. J., & Mehler, P. S. (2020). Medical complications of anorexia nervosa. Cleveland Clinic Journal of Medicine, 87(6), 361–366. Sylvester, C. J., & Forman, S. F. (2008). Clinical practice guidelines for treating restrictive eating disorder patients during medical hospitalization. Current Opinion in Pediatrics, 20(4), 390–397. Udo, T., & Grilo, C. M. (2019). Psychiatric and medical correlates of DSM-5 eating disorders in a nationally representative sample of adults in the United States. International Journal of Eating Disorders, 52(1), 42–50. Fagin, L. (2004). Management of personality disorders in acute in-patient settings. Part 1: Borderline personality disorders. Advances in Psychiatric Treatment, 10(2), 93–99.

