Diversity, Equity, and Inclusion
Session: Poster Session
(070) Mutism, Mutilation, and Marginalization: Coordinated Care for a Transgender Female
Trainee Involvement: Yes

Hilary Linzie Massey, MD
Associate Program Director, Assistant Professor
Kirk Kerkorian School of Medicine at UNLV
Las Vegas, Nevada, United States- ZL
Zachary Leavitt, BS
Student
Kirk Kerkorian School of Medicine at UNLV
Las Vegas, Nevada, United States - CO
Crystal M. Oden, n/a
Medical Student
Kirk Kerkorian School of Medicine at UNLV
Henderson, Nevada, United States
Presenting Author(s)
Co-Author(s)
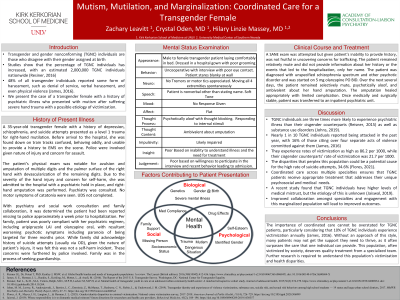
Transgender and gender nonconforming (TGNC) individuals are those who disagree with their gender assigned at birth. Studies have shown that the percentage of TGNC individuals has increased, with an estimated 2,000,000 TGNC individuals nationwide (Resiner, 2016). In a national survey, 48% of all transgender individuals reported some form of harassment, such as denial of service, verbal harassment, and even physical violence (James, 2016). We present a case report of a transgender female with a history of psychiatric illness who presented with mutism after suffering severe hand trauma with a possible etiology of victimization. Case Report A 35-year-old transgender female with a history of depression, schizophrenia, and suicide attempts presented as a level 1 trauma activation for right-hand mutilation. Patient was found by EMS near railroad tracks, disoriented, and unable to provide basic history. A hand amputation was performed. Psychiatric evaluation found her experiencing psychotic and trauma symptoms, remaining mute during hospitalization. No catatonia was seen. Appropriate psychotropics were initiated, she was medically stabilized and managed post-operatively by surgery. Social services was able to locate her family, who reported that the patient was missing prior to hospitalization. Collateral provided by family led us to believe there was a concern for patient victimization, including trafficking versus self-inflicted injury. A coordinated effort between trauma surgery, social work, psychiatry, internal medicine, and hand surgery allowed the patient to be safely transferred for inpatient psychiatric care. Discussion TGNC individuals are three times more likely to experience psychiatric illness than their cisgender counterparts (Reisner, 2015). A national survey found that nearly one in ten TGNC individuals reported being attacked in the past year, with 16% of those citing over four separate acts of violence committed against them (James, 2016). Coordinated care across multiple specialties ensures that TGNC patients receive appropriate treatment that addresses their unique needs and concerns. Care for this population requires much more than medical treatment; providers must be emotional and societal support systems. Conclusion The importance of coordinated care cannot be overstated for TGNC patients, particularly considering that 10% of TGNC individuals experience victimization annually (James, 2016). Without an approach of this style, many patients may not get the support they need to thrive. This population, often victimized by society, deserves quality treatment from a specialized team. Further research is required to understand this population's victimization and health disparities. 1. Reisner SL, Dr, Poteat T, PhD, Keatley J, MSW, et al. Global health burden and needs of transgender populations: A review. The Lancet (British edition). 2016;388(10042):412-436. https://www.clinicalkey.es/playcontent/1-s2.0-S014067361600684X. doi: 10.1016/S0140-6736(16)00684-X. 2. James, S. E., Herman, J. L., Rankin, S., Keisling, M., Mottet, L., & Anafi, M. (2016). The Report of the 2015 U.S. Transgender Survey. Washington, DC: National Center for Transgender Equality 3. Reisner, Sari L., Sc.D., M.A, Vetters, Ralph, M.D., M.P.H, Leclerc M, M.P.H, et al. Mental health of transgender youth in care at an adolescent urban community health center: A matched retrospective cohort study. Journal of adolescent health. 2015;56(3):274-279. https://www.clinicalkey.es/playcontent/1-s2.0-S1054139X14006934. doi: 10.1016/j.jadohealth.2014.10.264.
Introduction:
References:

