Psycho-Oncology and Palliative Care
Session: Poster Session
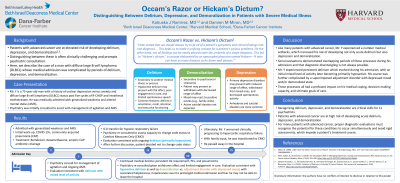
(123) Occam's Razor or Hickam's Dictum? Distinguishing between Delirium, Depression, and Demoralization in Patients with Severe Medical Illness
Trainee Involvement: No
- KR
Katiuska Ramirez, MD
Associate Director, Psychiatric Consultation-Liaison Service
Beth Israel Deaconess Medical Center
Boston, Massachusetts, United States 
Damien Miran, MD
Clinical Director, DFCI Inpatient Psychiatry Consult Service
Dana-Farber Cancer Institute
Boston, Massachusetts, United States
Presenting Author(s)
Co-Author(s)
Mr. Y is a 75-year-old man with a history of unspecified depression and severe DLBCL who was admitted for management of generalized weakness and altered mental status. Initial work-up identified positive COVID-19 infection and concern for community-acquired pneumonia (CAP) for which he received remdesivir, dexamethasone, and empiric CAP antibiotic coverage. Psychiatry was consulted to assist with evaluation and management of impulsivity and agitation. Initial psychiatric evaluation was consistent with delirium secondary to multiple etiologies and chronic risk factors. Soon after admission, Mr. Y developed hypoxic respiratory failure requiring ICU transfer. Psychiatry was re-consulted due to patient’s limited engagement in medical care and to assess his decision-making capacity to change his code status to “comfort measures only.” Psychiatric evaluation in the ICU demonstrated ongoing delirium. Ultimately, Mr. Y decided not to change his code status. Four weeks later, Mr. Y reported depressed mood and anxiety secondary to worries about the future. During interview, he reported visual hallucinations and expressed vague death wishes without suicidal ideation. At this point, he was not a candidate for additional chemotherapy. Psychiatric evaluation at this time was consistent with hypoactive delirium with concern for adjustment disorder and/or element of demoralization. Additional goals-of-care discussions were held to explore patient’s treatment preferences. Like many patients with advanced cancer, Mr. Y experienced number medical setbacks which increased his risk of developing not only acute delirium but also depression and demoralization. For Mr. Y, serial evaluations demonstrated concern that he likely experienced each of these processes during his admission. While efforts to distinguish between these processes should be undertaken, patients like Mr. Y demonstrate that such diagnostic disentangling is not always possible. Losing sight of this diagnostic complexity can negatively impact patient care. In Mr. Y’s case, missing a diagnosis of delirium in the ICU may have led to a premature change in his code status. Likewise, ignoring demoralization and fixating on delirium may have prevented additional goals-of-care discussions later in his course. Conclusion/Implications: Recognizing delirium, depression, and demoralization are critical skills for CL psychiatrists. For many patients with advanced cancer, proper diagnostic evaluations must recognize the potential for these conditions to occur simultaneously and avoid rigid assessments which impede a patient’s treatment course. 1. Wein, Sulkes, A., & Stemmer, S. (2010). The Oncologist's Role in Managing Depression, Anxiety, and Demoralization With Advanced Cancer. The Cancer Journal (Sudbury, Mass.), 16(5), 493–499. https://doi.org/10.1097/PPO.0b013e3181f28b64. 2. Sánchez-Hurtado, L. A., Hernández-Sánchez, N., Del Moral-Armengol, M., Guevara-García, H., García-Guillén, F. J., Herrera-Gómez, Á., & Ñamendys-Silva, S. A. (2018). Incidence of Delirium in Critically Ill Cancer Patients. Pain research & management, 2018, 4193275. https://doi.org/10.1155/2018/4193275.
Background:
Patients with advanced cancer are at elevated risk of developing delirium, depression, and demoralization1,2. It is often difficult to distinguish between these processes. Here, we describe the case of a man with severe diffuse large B-cell lymphoma (DLBCL) with medical admission complicated by periods of delirium, depression, and demoralization, each of which impacted decisions related to his treatment plan.
Case Presentation:
Discussion:
References:

